When you get the flu, COVID-19, or hepatitis C, your body fights back-but sometimes it needs help. That’s where antiviral medications come in. Unlike antibiotics that kill bacteria, antivirals don’t destroy viruses. Instead, they mess with how viruses copy themselves, slowing them down enough for your immune system to catch up. The goal isn’t always to wipe out the virus completely, but to reduce symptoms, prevent hospital stays, and stop you from passing it to others.
How Antivirals Actually Work
Viruses can’t reproduce on their own. They hijack your cells and turn them into virus factories. Antivirals step in at different points in that process. Some block the virus from entering cells. Others stop it from copying its genetic material. Some interfere with how new virus particles are assembled.
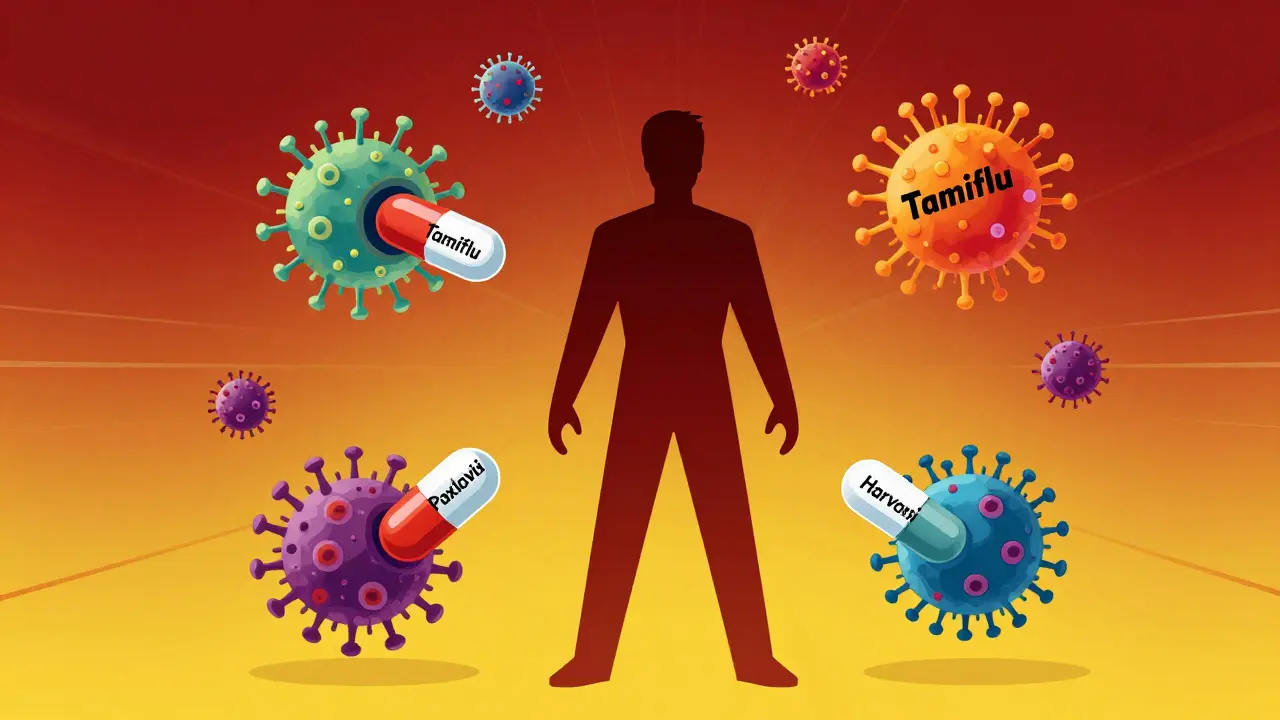
For example, oseltamivir (Tamiflu) works against the flu by blocking an enzyme called neuraminidase. Without it, new flu viruses can’t escape infected cells to spread. Paxlovid (nirmatrelvir/ritonavir), used for COVID-19, disables a key viral enzyme called protease, which the virus needs to make functional proteins. Without it, the virus can’t mature.
These drugs are highly specific. One antiviral won’t work for every virus. That’s why you can’t just take a flu pill for COVID or herpes. Each drug is designed to target a particular virus or family of viruses.
Top Antiviral Drugs for Common Infections
Here’s what’s actually being used today-and how well it works.
Influenza (Flu)
The CDC recommends four antivirals for flu: oseltamivir (Tamiflu), zanamivir (Relenza), peramivir (Rapivab), and baloxavir (Xofluza). If you start taking one within 48 hours of symptoms, you can shorten your illness by about a day or two. That might not sound like much, but for someone over 65 or with heart disease, it can mean the difference between recovering at home and ending up in the ICU.
But there’s a catch. Zanamivir (Relenza) is an inhaler-and it can trigger breathing problems in people with asthma or COPD. That’s why doctors often pick oseltamivir instead for those patients.
COVID-19
Paxlovid is the gold standard for high-risk patients. In clinical trials, it cut hospitalizations by 89% when taken within five days of symptoms. But it’s not perfect. About 60% of users report a strange metallic taste-nicknamed “Paxlovid mouth.” Some people also experience viral rebound: symptoms come back after finishing the course. That happens in about 10-15% of cases, according to the New England Journal of Medicine.
Molnupiravir (Lagevrio) is an alternative, but it’s less effective-only a 30% reduction in hospitalization. It’s usually only used when Paxlovid can’t be taken, like if you’re on blood thinners or statins that interact dangerously with ritonavir, the booster in Paxlovid.
Hepatitis C
This is where antivirals have changed everything. Before 2011, treatment meant weekly injections of interferon and daily pills of ribavirin for up to a year. Side effects were brutal: fatigue, depression, flu-like symptoms. Cure rates? Only 40-80%.
Now, direct-acting antivirals (DAAs) like Harvoni, Epclusa, and Mavyret are taken as one pill a day for just 8-12 weeks. Cure rates? 95-99%. No shots. No severe side effects. Most people don’t even notice they’re on medication.
HIV
Thirty years ago, an HIV diagnosis meant a death sentence. Now, with combination therapy-usually two nucleoside reverse transcriptase inhibitors (NRTIs) plus an integrase inhibitor-people with HIV can live just as long as anyone else. Drugs like tenofovir, emtricitabine, and dolutegravir suppress the virus so well that many patients have undetectable viral loads. That also means they can’t transmit the virus sexually.
Even newer options like Cabenuva let patients get a shot every month or two instead of taking pills daily. It’s a game-changer for adherence.
Why Timing Matters
Antivirals aren’t like painkillers you can take anytime. They work best when you start them early-usually within the first few days of symptoms.
For flu, that’s 48 hours. For COVID-19, it’s five days. For shingles, it’s 72 hours. After that, the virus has already spread too far. The medication might still help a little, but the biggest benefit is lost.
That’s why many doctors now give patients a prescription at the first sign of illness, even before test results come back. If the test is positive, they start. If it’s negative, they stop. It’s a simple trick that saves lives.
Biggest Challenges with Antivirals
Even the best drugs have limits.
Drug interactions are a huge problem. Paxlovid’s ritonavir component blocks a liver enzyme (CYP3A4) that breaks down dozens of common medications. That includes statins for cholesterol, blood thinners like apixaban, and even some anxiety meds. Up to 30% of older adults with multiple health conditions can’t take Paxlovid because of these conflicts.
Narrow targeting is another issue. Most antivirals work against one virus or a close relative. There’s no “universal antiviral” yet. That’s why we need new pills for every new virus-like we did with COVID-19. Experts are working on broad-spectrum antivirals, but none are ready for widespread use.
Resistance is a growing concern. Just like with antibiotics, viruses can mutate and become resistant. That’s why HIV treatment always uses combinations of drugs-it’s harder for the virus to dodge multiple attacks at once.
Who Gets Access? The Inequality Problem
These drugs save lives-but not everyone can get them.
In the U.S., only 38% of high-risk patients who qualified for Paxlovid actually got it in early 2023. Why? Pharmacists ran out. Doctors didn’t know how to prescribe it. Insurance didn’t cover it. In a Kaiser Family Foundation survey, 34% of eligible patients said they couldn’t get it due to supply or access issues.
It’s worse globally. The WHO says less than 5% of eligible patients in low-income countries received COVID-19 antivirals. Meanwhile, wealthy nations stockpiled them. This isn’t just unfair-it’s dangerous. Viruses don’t care about borders. When they spread unchecked anywhere, they mutate everywhere.

What’s Next?
The future of antivirals is exciting-and complicated.
CRISPR-based therapies are being tested to cut viral DNA out of human cells, aiming for a true cure for HIV. Long-acting injectables are replacing daily pills. New oral drugs for flu and RSV are in late-stage trials.
But the biggest hurdle isn’t science-it’s access. Until antivirals are affordable, available, and easy to prescribe everywhere, their potential will remain locked away.
What You Should Know
If you’re at risk for severe viral illness-older, diabetic, immunocompromised, or have heart or lung disease-talk to your doctor now. Don’t wait until you’re sick.
Ask: “If I get COVID or the flu, what antiviral can I get ahead of time?” Get the prescription filled and keep it at home. Know the signs to watch for. Start it early if you test positive.
Antivirals aren’t magic. They’re tools. And like any tool, they only work if you have them when you need them.
Can antiviral medications cure viral infections completely?
Some yes, most no. Hepatitis C can be cured in 95-99% of cases with direct-acting antivirals. HIV can be suppressed to undetectable levels, making it non-transmissible and manageable for life. But for flu, colds, and most other viruses, antivirals reduce severity and duration-they don’t eliminate the virus entirely. The immune system still does the final cleanup.
How long do antiviral medications take to work?
Most start working within hours, but you won’t feel better immediately. For flu, symptoms may improve in 1-2 days. For COVID-19, people often report feeling less fatigued or feverish within 24-48 hours of starting Paxlovid. The key is that they prevent worsening, not just relieve symptoms.
Are there side effects to antiviral drugs?
Yes, but they’re usually mild. Paxlovid can cause altered taste, diarrhea, or high blood pressure. Oseltamivir may cause nausea or vomiting. Hepatitis C drugs are often well-tolerated, with just mild fatigue. Serious side effects are rare. The bigger risk is drug interactions-especially with Paxlovid-so always tell your doctor what else you’re taking.
Can I take antivirals to prevent getting sick?
Only in rare cases. Baloxavir (Xofluza) is approved for post-exposure prevention of flu in people over 12. It’s not for routine use. There’s no approved antiviral to prevent COVID-19 before exposure. Vaccines are still the best prevention tool. Antivirals are for treatment, not prevention.
Why isn’t Paxlovid prescribed more often?
Three main reasons: drug interactions (it can’t be taken with many common meds), limited supply early in the pandemic, and lack of provider awareness. Many doctors didn’t know how to screen for interactions or didn’t realize how effective it was. Now, tools like the University of Liverpool’s drug interaction checker help, but uptake still lags behind potential.
Do antivirals work against the common cold?
No. The common cold is caused by over 200 different viruses, mostly rhinoviruses. No antiviral has been proven effective against them. Rest, fluids, and symptom relief are the only recommended treatments. Don’t waste money on antiviral cold remedies-they don’t work.




13 Comments
Lana Kabulova-22 January 2026
Antivirals are amazing but why do we act like they’re magic bullets? I’ve seen people panic-buy Tamiflu like it’s toilet paper during a pandemic… and then never use it because they ‘waited too long’
shivani acharya-23 January 2026
Let’s be real-pharma companies invented antivirals so they could sell us a new pill every time a virus sneezes. They don’t want a cure, they want lifelong customers. That’s why Paxlovid has that weird taste-it’s a marketing ploy to make you remember it. And don’t get me started on the ‘viral rebound’… they knew this would happen. They just didn’t tell you.
Meanwhile, in India, we’re still waiting for our first dose of anything. But hey, at least the rich get their ‘Paxlovid mouth’ while the rest of us get the virus. Capitalism is beautiful.
And yes, I’ve read the NEJM. And the Lancet. And the WHO reports. And no, I’m not paranoid-I’m just informed.
They’re testing CRISPR for HIV? Cute. Meanwhile, my cousin in Mumbai got hepatitis C from a dirty needle at a clinic and was told to ‘wait and see.’
Don’t tell me about ‘access.’ This isn’t a public health issue. It’s a profit issue. And the next pandemic? They’ll be ready-with a $2,000 pill you can’t afford.
Brenda King-25 January 2026
I love how this post breaks down the science without jargon. As a nurse, I’ve seen too many elderly patients skip antivirals because they think ‘it’s just a cold.’ But flu can kill someone with COPD in 72 hours. Please, if you’re over 65 or have a chronic condition-get that prescription now. Don’t wait until you’re gasping.
Also, Paxlovid’s metallic taste? Yeah, it’s gross. But I’ve had patients say, ‘I’d take that taste every day if it kept me out of the hospital.’
And yes, drug interactions are a nightmare. I had to call three pharmacies before I found one that had the interaction checker up to date. We’re not just treating viruses-we’re playing Tetris with prescriptions.
And if you think antivirals are for prevention? Nope. Vaccines are. Please stop asking your doctor for ‘a little Paxlovid just in case.’
Also, thank you for mentioning Hep C. That’s the real miracle. One pill a day. No shots. 99% cure rate. We should be screaming about this from rooftops.
And to those saying ‘why not just boost immunity?’-antivirals don’t replace your immune system. They give it a fighting chance. You’re not weak for taking them. You’re smart.
Also, I keep a script for Tamiflu in my medicine cabinet. Just in case. And I tell everyone I know to do the same. It’s not paranoia. It’s preparedness.
And yes, I’ve had patients cry because they couldn’t get Paxlovid. Not because they were sick. Because they were scared. And that’s the real tragedy.
Thanks for writing this. It’s the kind of post that saves lives. ❤️
Keith Helm-26 January 2026
Antivirals are not prophylactic. They are therapeutic. The distinction is critical.
Alec Amiri-27 January 2026
People are still taking Tamiflu? That’s like using a flip phone in 2024. Baloxavir is way better-single dose, no nausea, works in 24 hours. Why are doctors still prescribing the old stuff? Lazy. Or they just don’t read journals.
And Paxlovid? Yeah, it’s great. But 60% taste weird? That’s not a side effect-that’s a red flag. If your mouth tastes like a battery, something’s wrong. And viral rebound? That’s not ‘rebound’-that’s the virus laughing at us.
Also, why is no one talking about how we’re still using 1980s-era flu drugs? We’ve had 20 years of research. Why are we still stuck with neuraminidase inhibitors? Because Big Pharma doesn’t want to replace a cash cow with a better pill.
And don’t get me started on Hep C. Yeah, it’s a miracle. But the price? $80,000 a course. In the U.S. That’s not medicine. That’s extortion.
Neil Ellis-28 January 2026
Man, this post gave me chills. I remember when HIV was a death sentence. My brother was diagnosed in ’98. We thought we’d bury him by 2002. Now? He’s hiking the Rockies, teaching yoga, and his viral load is undetectable. Antivirals didn’t just save his life-they gave him back his future.
And Hep C? My cousin in Texas was a junkie for 12 years. Got infected. Thought she was doomed. Took Harvoni for 12 weeks. Now she’s a peer counselor for addicts. No scars. No shame. Just life.
It’s not magic. It’s science. And it’s beautiful.
But yeah… access is broken. I’ve seen nurses cry because they had the meds but the patient’s insurance denied it. That’s not healthcare. That’s a moral failure.
Let’s not just celebrate the science. Let’s fight for the people who need it.
And hey-if you’re reading this and you’re over 50? Talk to your doc. Get that script. Don’t wait until you’re on oxygen. Be the person who’s ready.
We’ve got the tools. Let’s make sure no one’s left behind. 🌍❤️
Patrick Roth-29 January 2026
Actually, you’re all wrong. Antivirals don’t work at all. Viruses are just a government tool to control the population. The ‘viral rebound’? That’s not the virus-it’s the placebo effect kicking in after you stop the pills. And ‘Paxlovid mouth’? That’s just your body rejecting the nanotech in the drug. They’ve been embedding microchips in meds since 2017. You think the taste is bad? Wait till you see the tracking logs.
Also, Hep C cure rates? Fabricated. The real cure is fasting and drinking lemon water. I’ve seen it. I’m from Ireland. We know about healing.
And why do you think they push vaccines? To make you dependent on antivirals. It’s a cycle. A profit cycle. Wake up.
Liberty C-30 January 2026
It’s astonishing how casually this article dismisses the systemic failures in pharmaceutical distribution. To frame antivirals as ‘tools’ is to ignore the fact that tools require infrastructure-and in the U.S., that infrastructure is stratified by zip code, income, and insurance tier. The notion that ‘getting a prescription ahead of time’ is a viable strategy for the uninsured or underinsured is not just naive-it’s cruel.
And the romanticization of ‘one pill a day’ for Hep C ignores the fact that these drugs were priced at $1,000 per tablet in 2014. Only after public outrage and litigation did prices drop. This is not progress. It’s corporate damage control.
CRISPR? Long-acting injectables? All fascinating. But until we dismantle the profit-driven model of medicine, these innovations will remain luxury goods for the privileged few.
And let’s not pretend that ‘Paxlovid mouth’ is a trivial side effect. It’s a metaphor: the taste of inequity.
arun mehta-31 January 2026
As someone from India, I’ve seen both sides. My uncle got Hep C treatment in Delhi-$200 for 12 weeks. Full cure. No drama. No insurance battles. Because India makes generic DAAs. And yes, they’re just as effective.
So when people say ‘antivirals are too expensive,’ I say: they’re only expensive if you’re buying them from the U.S. pharma giants.
Global access isn’t about charity. It’s about justice. And science should never be a privilege.
Also, I keep a copy of the CDC guidelines on my phone. I share it with my family. And my neighbors. Because knowledge is the real antiviral.
And yes-I use emojis. 😊🙏
Daphne Mallari - Tolentino- 1 February 2026
One must observe with clinical precision that the efficacy of antiviral agents is contingent upon the temporal window of intervention-a principle that is both empirically validated and biologically logical. To suggest that antivirals function as panaceas is to misunderstand the fundamental virological paradigm.
Furthermore, the assertion that ‘access’ is the primary barrier is both reductive and ideologically charged. The issue is not merely distribution-it is the confluence of regulatory fragmentation, pharmacoeconomic policy, and provider education.
One cannot, in good conscience, advocate for universal access without first acknowledging the complexity of the supply chain, the legal constraints on off-label prescribing, and the limitations of current diagnostic infrastructure.
It is not enough to say ‘get the script.’ One must also ask: who has the bandwidth to navigate the bureaucracy?
Chiraghuddin Qureshi- 2 February 2026
Love this post! 🙌 From Delhi to New York, we all just want to stay healthy. Antivirals are like a fire extinguisher-you hope you never need it, but when you do, you’re so glad it’s there.
My aunt in Mumbai took the Hep C pills. No side effects. Just slept more. Then boom-cured. No drama.
And yeah, Paxlovid tastes like a battery. But I’d eat a whole pack if it saved my dad. 😅
Thanks for the real talk. 🌏❤️
Rob Sims- 2 February 2026
Wow. Just… wow. You wrote a 2,000-word essay and still missed the point. Antivirals don’t cure anything. They just delay death so Big Pharma can sell you another pill next year. You think that’s progress? That’s slavery with a prescription.
And don’t give me that ‘get the script’ nonsense. You think your doctor actually cares? They’re paid per visit. They don’t want you healthy. They want you coming back.
And vaccines? Yeah, right. They’re just a gateway drug to antivirals. You’re being played.
Wake up. The system is rigged. And you’re the mark.
Brenda King- 4 February 2026
And to the person who said ‘antivirals are a scam’-I’ve held the hands of people dying from flu because they didn’t get Tamiflu in time. You don’t get to say that from your keyboard while breathing clean air.
My grandmother died in 2020 because she couldn’t get Paxlovid. She was 78. Had diabetes. Wasn’t rich. Didn’t have a doctor who knew how to prescribe it.
So no. This isn’t about ‘the system.’ It’s about people. Real people. Who just wanted to live.
Don’t be a cynic. Be a helper.
And if you’re reading this and you’re healthy? Talk to your doctor. Get the script. Keep it in your drawer.
One day, you’ll thank yourself.