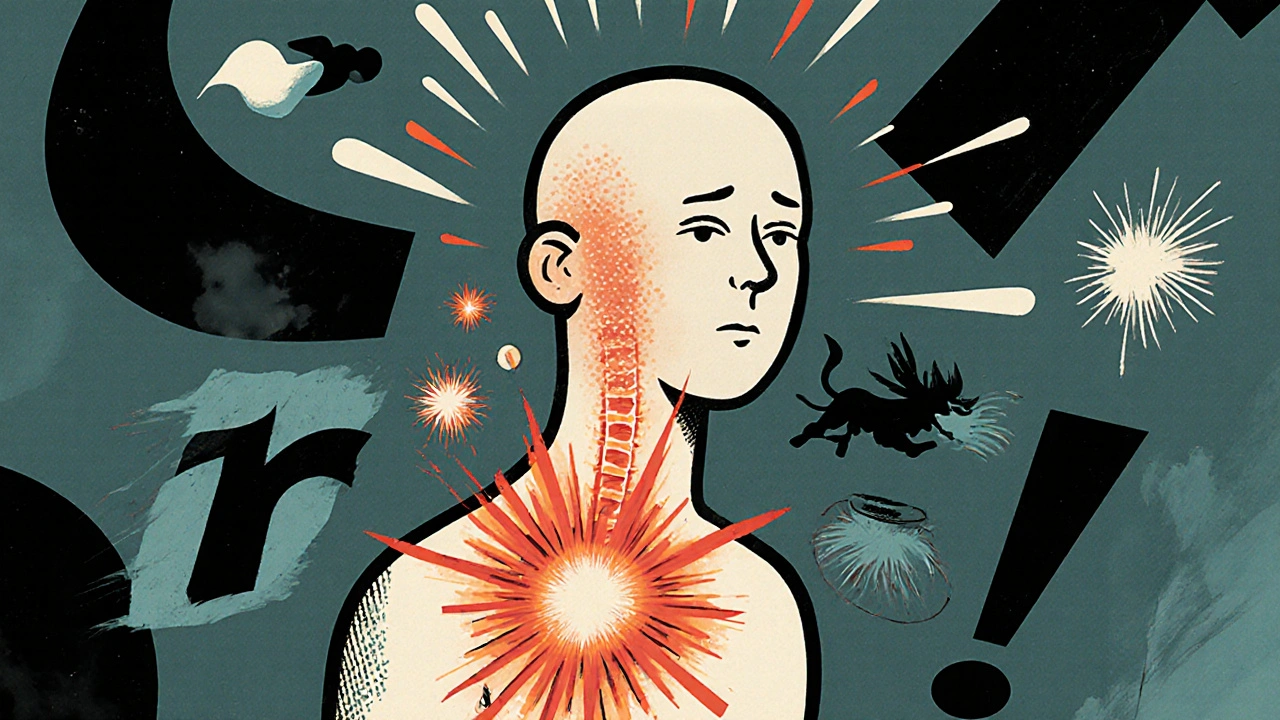
Imagine touching a doorknob and feeling like your skin is on fire. Or getting a hug that hurts more than a punch. If you’ve ever had pain that doesn’t make sense-pain that spreads, gets worse with light touch, or lingers long after an injury healed-you’re not imagining it. You might be experiencing central sensitization.
What Exactly Is Central Sensitization?
Central sensitization isn’t just pain. It’s your nervous system turning up the volume on pain signals until even quiet whispers sound like screams. It happens when your brain and spinal cord become hyper-sensitive, reacting to normal signals as if they’re dangerous. This isn’t a sign of weakness or mental health issues. It’s a real, measurable change in how your nervous system works.Back in 1983, neuroscientist Clifford J. Woolf first described this phenomenon as a "spinal cord wind-up." Think of it like a volume knob stuck on max. Normally, your body sends pain signals only when something’s actually damaged-like a cut or a sprain. But with central sensitization, your nervous system starts reacting to things that shouldn’t hurt at all. A light brush of fabric, a breeze, even a routine touch during a doctor’s exam can trigger intense pain.
This isn’t rare. About 2-4% of people worldwide have chronic pain conditions driven by central sensitization. That’s tens of millions of people. Conditions like fibromyalgia, chronic low back pain lasting more than three months, and some types of migraines are strongly linked to it. In fact, up to 90% of people with fibromyalgia show clear signs of central sensitization.
How Does Your Nervous System Get Like This?
Your nervous system is designed to adapt. It learns. And sometimes, it learns the wrong thing. When you have repeated or long-lasting pain-say, from an old injury, a surgery, or even a viral infection-your spinal cord and brain start changing. Neurons become more excitable. Inhibitory pathways that normally calm down pain signals weaken. Chemicals like cytokines and norepinephrine spike, creating a feedback loop of heightened sensitivity.Studies using fMRI show that people with central sensitization have 20-35% more activity in brain areas that process pain. Their pain circuits are literally rewired. At the same time, their body’s natural painkillers-like endogenous opioids-become less effective. Mu-opioid receptor binding drops by 15-25%, meaning your body’s own pain-relief system is struggling to keep up.
It’s not just about the nerves. Immune activity plays a role too. Up to 65% of people who develop chronic pain after a viral illness show signs of immune-driven sensitization. Even stress and poor sleep can make it worse, because they keep your nervous system in overdrive.
What Does It Feel Like?
If you’ve got central sensitization, your pain doesn’t follow the rules. Here’s what it typically looks like:- Widespread pain-affects multiple body areas, not just where you were injured. You might have pain in your neck, knees, and hands, even if you only hurt your back.
- Allodynia-pain from things that shouldn’t hurt. Light clothing, a bedsheet, or even a fan blowing on your skin can feel painful.
- Hyperalgesia-normal pain feels much worse. A slight bump on the arm might feel like a bruise that lasts for days.
- Temporal summation-repeated light touches build up into intense pain. That’s the "wind-up" effect Woolf described.
Many people also report "brain fog," trouble sleeping, and sensitivity to light, noise, or smells. It’s not just pain-it’s your whole system being overloaded. Reddit threads from people with fibromyalgia are full of stories like: "I can’t wear a watch because the band hurts," or "My partner’s hand on my shoulder feels like needles."
How Is It Diagnosed?
There’s no single blood test or X-ray for central sensitization. Doctors use a mix of clinical signs and tests:- Pain drawings: If your pain map covers areas far from your original injury, it’s a red flag.
- Quantitative Sensory Testing (QST): This measures your pain threshold. People with central sensitization often feel pain at 20-30% lower pressure than normal.
- Conditioned Pain Modulation (CPM): This test checks how well your body can turn off pain. In central sensitization, this system is 40-50% weaker.
One of the biggest challenges? Many doctors still don’t recognize it. A 2023 survey found only 65% of clinicians agree on whether a patient has it. Orthopedic surgeons diagnose it in just 25% of chronic pain cases, while rheumatologists catch it in 65% of fibromyalgia patients. That mismatch leads to long delays-63% of patients see 4 to 6 doctors over 2 to 5 years before getting the right diagnosis.
How Is It Different From Other Types of Pain?
Not all chronic pain is the same. Here’s how central sensitization stands out:| Feature | Peripheral Nociceptive Pain | Neuropathic Pain | Central Sensitization |
|---|---|---|---|
| Location | Follows anatomy (e.g., herniated disc → leg pain) | Dermatomal (follows nerve pathways) | Widespread, non-anatomical |
| Pain Duration | Resolves in 6-12 weeks after healing | Can last long-term, but localized | Often lasts 14+ months, even without tissue damage |
| Trigger | Physical injury or inflammation | Nerve damage | Repeated signals, stress, infection |
| Pain Intensity (avg) | 4.2/10 | 6.1/10 | 7.8/10 |
| Best Treatment | Anti-inflammatories, rest | Anticonvulsants, lidocaine patches | SNRIs, gabapentinoids, pain education |
Unlike neuropathic pain-which usually follows a nerve’s path-central sensitization doesn’t care about anatomy. It can show up in your foot, your head, and your chest all at once. And unlike simple tissue damage, it doesn’t fade when the injury heals. That’s why so many people are told, "It’s all in your head." But it’s not. It’s in your nervous system.

What Treatments Actually Work?
The good news? Central sensitization can improve. It’s not permanent. The nervous system can unlearn this overdrive state-especially when you remove the triggers and retrain it.Medications:
- Pregabalin (Lyrica): 300-1200mg daily helps 55% of patients reduce pain by 30-50%.
- Duloxetine (Cymbalta): 60mg daily leads to 30% pain reduction in 45% of users.
- Low-dose naltrexone (LDN): 4.5mg nightly improves symptoms in 40% of fibromyalgia patients.
- Nortriptyline: 25-50mg at night helps with sleep and pain in nearly half of users.
These aren’t painkillers like opioids. They work by calming overactive nerves and restoring balance in the central nervous system.
Non-drug approaches:
- Pain neuroscience education: Teaching patients how their nervous system works reduces fear and catastrophizing. Studies show 20-30% improvement in pain-related anxiety after just a few sessions.
- Graded exercise: Start slow-10% increase in activity per week. Walking, swimming, or cycling builds tolerance without triggering flare-ups. Functional improvement: 25-40%.
- Mindfulness and stress reduction: An 8-week program can lower pain interference scores by 25%. This isn’t "just relaxing." It’s literally changing how your brain processes threat signals.
One of the biggest barriers? Side effects. About 35-45% of people stop meds because of dizziness, fatigue, or nausea. That’s why combining meds with non-drug strategies works best.
Why This Matters Now
The global market for treatments targeting central sensitization is projected to hit $28.3 billion by 2028. Research funding from the NIH has grown 50% since 2018. More pain centers now include sensory testing in their protocols. And new biomarkers-like elevated substance P in spinal fluid or reduced mu-opioid binding on PET scans-are making diagnosis more precise.But the real breakthrough isn’t a drug. It’s understanding. When people realize their pain isn’t "all in their head," but a real, biological change in their nervous system, it changes everything. They stop blaming themselves. They stop feeling broken. They start taking back control.
What’s Next?
Researchers are working on drugs that target specific molecules involved in sensitization. Five compounds are already in Phase II trials. By 2027, diagnostic tools aim to hit 90% accuracy. And by 2026, half of physical therapy programs plan to teach pain neuroscience to patients.For now, the most powerful tool you have is knowledge. If you’ve had unexplained, widespread, or exaggerated pain for months or years, ask your doctor about central sensitization. Bring this info. Ask about QST or CPM testing. Don’t settle for being told it’s psychological. Your pain is real. Your nervous system is just stuck on high.
Recovery isn’t about eliminating pain overnight. It’s about retraining your system. It takes time. But with the right approach, many people find their pain drops significantly-and their lives get back.
Is central sensitization the same as fibromyalgia?
No, but they’re closely linked. Fibromyalgia is a diagnosis based on symptoms like widespread pain and fatigue. Central sensitization is the underlying mechanism-how the nervous system processes pain. About 90% of fibromyalgia patients have central sensitization, but not everyone with central sensitization has fibromyalgia. It can also occur in chronic low back pain, migraines, or after surgery.
Can central sensitization go away?
Yes. Unlike nerve damage, which is often permanent, central sensitization is a learned response. When the nervous system stops being bombarded by pain signals and starts receiving new, safe input-through exercise, education, and stress reduction-it can reset. Many people report major improvements after 6-12 months of consistent, gentle treatment.
Why do some doctors not believe in central sensitization?
Because it’s invisible on X-rays or blood tests. Until recently, medical training focused on structural damage as the source of pain. Many doctors still think if there’s no "damage," there’s no real pain. But brain scans and sensory testing now prove the changes are real. Awareness is growing, but it’s slow. Don’t let a doctor’s lack of knowledge make you doubt your experience.
Are opioids helpful for central sensitization?
No, and they often make it worse. Central sensitization involves reduced effectiveness of the body’s natural opioid system. Adding external opioids doesn’t fix this-it can make the nervous system even more sensitive over time. Studies show opioids have little benefit for fibromyalgia or widespread pain and carry high risks of dependence and worsening pain.
Can stress cause central sensitization?
Stress doesn’t cause it alone, but it’s a major trigger and amplifier. Chronic stress keeps your nervous system in fight-or-flight mode, which lowers your pain threshold and reduces your body’s ability to shut off pain signals. Many people notice flare-ups during high-stress periods. Managing stress isn’t optional-it’s part of treatment.
What should I avoid if I have central sensitization?
Avoid sudden, intense activity, extreme heat or cold, and anything that triggers a flare-up without gradual adaptation. Don’t push through pain. Avoid long periods of inactivity-movement, even gentle, is key. Also avoid dismissing your symptoms or letting others tell you it’s "just anxiety." Your pain is real, and your body needs gentle, consistent care.




14 Comments
Ross Ruprecht-22 November 2025
So let me get this straight-my back pain from lifting boxes is now a neuroscience PhD thesis? Cool. I’ll just stop taking ibuprofen and start meditating on my spinal cord’s volume knob.
Ragini Sharma-24 November 2025
lol i thought i was just weak but turns out my nerves are just too extra?? like why does my shirt collar feel like barbed wire?? also why does everyone act like this is new news?? i’ve been saying this since 2018
Javier Rain-26 November 2025
THIS. This is the most accurate breakdown I’ve ever seen. I’ve had fibro for 12 years and no doctor ever explained it like this. The part about mu-opioid receptors dropping? That’s why tramadol stopped working after 6 months. I’m printing this out and handing it to my new rheum. Thank you.
Bryson Carroll-27 November 2025
So what you’re saying is my chronic pain is just my brain being dramatic? Like if I just stopped being a baby it would go away? No wonder I’m broke and lonely. My nervous system is a diva and I’m the maid
Manjistha Roy-29 November 2025
As someone who has lived with this for over 15 years, I want to emphasize that this is not a diagnosis of weakness-it is a physiological reality. Many of us have been dismissed, misdiagnosed, and gaslit for years. The fact that QST and CPM are not standard in primary care is a systemic failure. Please, if you are a clinician reading this-learn this. Your patients are not lying.
Laurie Sala- 1 December 2025
Can we talk about how everyone says ‘it’s not in your head’ but then immediately talks about ‘rewiring your brain’? So… it IS in your head? And if your brain is the problem… isn’t that mental? I’m so confused now. Also I tried gabapentin and it made me feel like a zombie. Thanks for nothing.
Richard Wöhrl- 2 December 2025
Important clarification: central sensitization isn’t ‘just’ fibromyalgia-it’s a mechanism. I’ve seen it in post-surgical chronic pain, long-haulers from COVID, even after a bad case of shingles. The key is recognizing the pattern: widespread, non-anatomical, allodynia, and poor response to NSAIDs. If you’re seeing these signs, don’t stop at ‘depression’ or ‘anxiety.’ Push for QST. It’s not expensive, and it’s objective.
Matthew Mahar- 3 December 2025
My mom says I’m too sensitive but now I have a whole paper that says my nerves are just too loud?? I cried reading this. I’m not broken. I’m just wired wrong. Also I can’t wear jeans anymore. The seam feels like glass. I’m not dramatic. I’m just… sensitized.
Lisa Detanna- 4 December 2025
As an immigrant from a culture where pain is ‘endured silently,’ this article changed my life. My grandmother told me to ‘walk it off’ for 30 years. Now I know my body wasn’t weak-it was overwhelmed. I’m finally starting physical therapy with a pain specialist. Thank you for validating what I couldn’t say.
Lisa Lee- 6 December 2025
Ugh. Another American medical overcomplication. In Canada we just say ‘chronic pain’ and give you a TCA and a hug. Why do you need fMRI scans to know your body hurts? We don’t need to turn pain into a TED Talk.
Adrian Rios- 6 December 2025
Let me be real-this isn’t just about pain. It’s about being believed. I’ve been told I’m lazy, depressed, anxious, a hypochondriac, a malingerer. I’ve lost jobs, friendships, relationships because no one could see the storm inside my nervous system. This isn’t just science-it’s dignity. If you’re reading this and you’ve been told it’s ‘all in your head,’ you’re not crazy. You’re just stuck in a system that still thinks pain needs to show up on an X-ray to be real. I’m not asking for pity. I’m asking for recognition. And now, at least, I have this to show them.
Casper van Hoof- 7 December 2025
One must contemplate the phenomenological rupture between nociception and suffering. The Cartesian dichotomy collapses when the body becomes a site of epistemological ambiguity. The nervous system, in its hyperplastic state, is not merely malfunctioning-it is redefining the ontological boundaries of sensation. Thus, to pathologize central sensitization is to reify the very medical gaze that has rendered the suffering subject invisible.
Demi-Louise Brown- 7 December 2025
For those new to this: start with 5 minutes of walking daily. Add 1 minute each week. Don’t push through pain. Rest when needed. Sleep hygiene matters more than you think. Medication helps, but consistency in movement and stress management is the foundation. You will have setbacks. That doesn’t mean you failed. It means your nervous system is learning. Be patient. You are not alone.
John Mackaill- 9 December 2025
Just wanted to say thanks to the OP. This is the first time I’ve seen a post that didn’t sound like a pharmaceutical ad or a self-help blog. The part about immune-driven sensitization after viral illness? That’s me. I had mono in 2017 and never stopped hurting. I didn’t know it had a name. I thought I was just unlucky. Now I have a direction. Thank you for making me feel seen.