Medication Safety Assessment Tool
Medication Safety Assessment
This tool helps you identify medications that might be candidates for deprescribing. Based on evidence from deprescribing.org and clinical guidelines, it assesses whether your medications are still appropriate for your current health status.
Note: This tool is for informational purposes only. Always discuss medication changes with your healthcare provider.
Every year, millions of older adults take medications that no longer help them-and may be hurting them. It’s not laziness or neglect. It’s inertia. A pill gets prescribed for a short-term issue, then keeps getting refilled year after year. A sleep aid becomes a nightly habit. A stomach acid reducer turns into a lifelong routine. But here’s the truth: deprescribing isn’t about stopping medicine. It’s about making smarter choices.
What Deprescribing Really Means
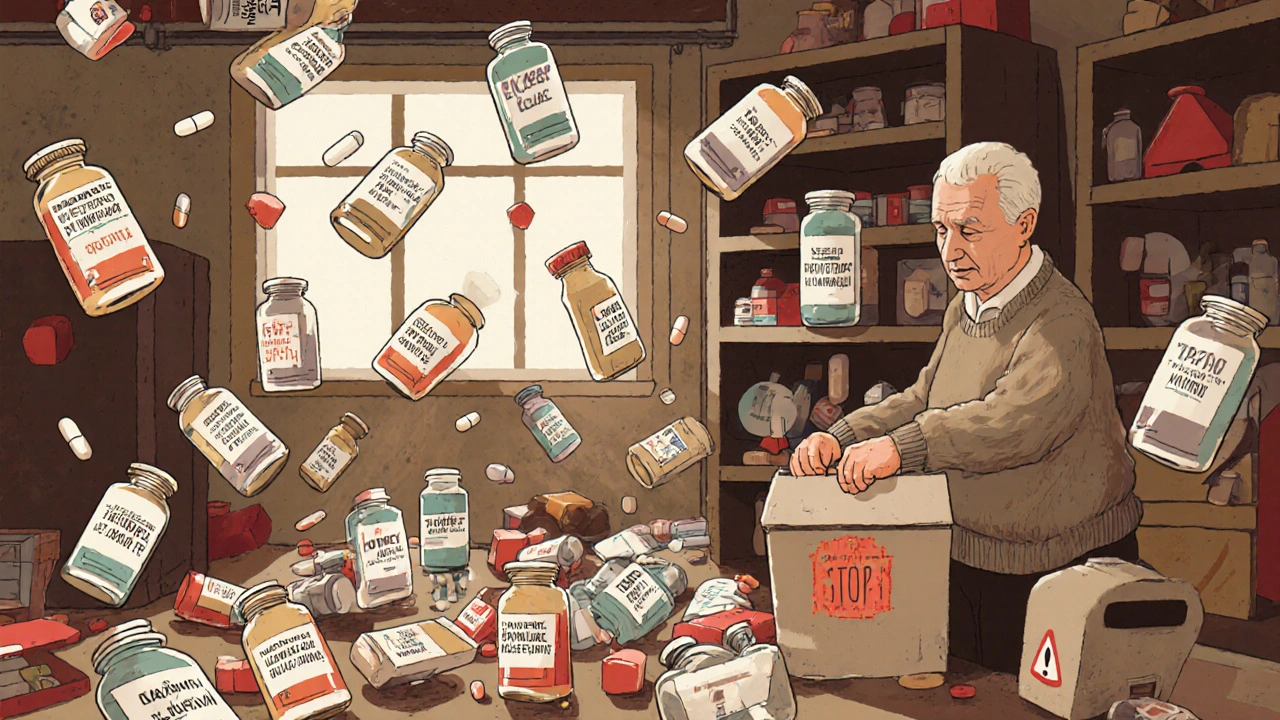
Deprescribing isn’t just cutting pills. It’s a deliberate, step-by-step process to review every medication a person is taking and decide: is this still helping, or is it just adding risk? Think of it like cleaning out a cluttered garage. You don’t throw everything away. You keep what’s useful, toss what’s broken, and store what you might need again-only if it’s safe to keep. In medicine, that means asking hard questions: Does this drug still match the patient’s current health? Are the side effects worse than the benefit? Could stopping it improve quality of life? The idea gained real traction around 2012, thanks to researchers in Canada like Barbara Farrell and Cara Tannenbaum. They didn’t just say, “Stop giving so many pills.” They built tools-frameworks-to make it safe, repeatable, and evidence-based. Today, deprescribing.org is the go-to resource for clinicians worldwide. And the data backs it up: about 40% of older adults globally are taking five or more medications, a situation called polypharmacy. That’s not normal. It’s risky.Why It Matters: The Hidden Cost of Too Many Pills
More pills don’t mean better health. They mean more falls, more confusion, more hospital trips. In fact, one in three hospital admissions for adults over 65 is linked to medication problems. That’s not a fluke. It’s a system failure. Take proton-pump inhibitors (PPIs), like omeprazole. These are often prescribed for heartburn. But if someone’s been on them for five years with no symptoms? The risks add up: lower bone density, kidney issues, infections. The guideline? Try to stop them. Taper slowly over 4 to 8 weeks. Monitor. Most people don’t need them anymore. Benzodiazepines-drugs like diazepam or lorazepam-are another big one. Used for anxiety or sleep, they can cause dizziness, memory loss, and falls. In older adults, even small doses increase fall risk by 50%. Yet many patients take them for years because “it’s what they’ve always done.” Antipsychotics are used off-label for agitation in dementia. But studies show they don’t fix the root problem-they just suppress behavior. And they raise the risk of stroke and death. The American Geriatrics Society says these drugs should be a last resort. The pattern is clear: many medications prescribed for one condition become harmful over time, especially when multiple drugs interact. And the longer they’re taken, the harder they are to stop.The Shed-MEDS Framework: A Proven Way to Cut Medications
Not all deprescribing is the same. Some doctors just guess. The best approach uses structured tools. One of the most validated is Shed-MEDS: Systematic History, Evaluate, Deprescribing, Enhance, Document, Support. It’s not a checklist. It’s a conversation. Here’s how it works:- Best Possible Medication History-Get the full list. Not what the patient remembers. Not what the chart says. What they’re actually taking, including supplements and over-the-counter drugs.
- Evaluate-Use tools like STOPP/START criteria (2021 version) or the Beers Criteria (2023 update) to flag potentially inappropriate meds.
- Deprescribing Recommendations-Prioritize. Which drugs carry the highest risk? Which are least effective now?
- Synthesis-Work with the patient. What are their goals? Do they want to feel clearer-headed? Walk without fear of falling? Sleep better without a pill?

Who Does This Best? Pharmacists and Nurses
Doctors are stretched thin. A typical visit lasts 7 to 10 minutes. There’s no time to review 12 medications, explain tapering, and address fears. But pharmacists? They’re trained for this. Medication Therapy Management (MTM) programs require over 150 hours of specialized training. In settings where pharmacists lead deprescribing-like long-term care homes or hospital discharge teams-medication reductions are 35% to 40% higher than in primary care. One pharmacist in Alberta, Canada, used the deprescribing.org benzodiazepine algorithm to help 18 out of 22 patients taper off safely. Only two had mild withdrawal. That’s success. Nurse practitioners and clinical pharmacists are also key. They spend time listening. They track symptoms. They follow up. They’re the ones who notice when a patient stops sleeping because they’re scared to stop their sleeping pill. Primary care doctors want to do this. But without support, they can’t. A 2022 study found fewer than 15% of primary care practices in Canada had formal deprescribing protocols. In the U.S., it’s even lower.Barriers: Why It’s Still Rare
The science is solid. The tools exist. So why isn’t everyone doing it? First, time. No one has enough of it. A full deprescribing review can take 45 minutes. That’s three patient visits. Second, fear. Patients are scared. “I’ve taken this for 15 years. What if I get worse?” Doctors are scared too. “What if I stop it and something bad happens?” Third, systems don’t help. Most electronic health records don’t flag medications for review. They don’t suggest tapering schedules. They don’t remind you to check if a drug is still needed. Some even auto-renew prescriptions. Fourth, guidelines are incomplete. There are solid deprescribing protocols for five drug classes: PPIs, benzodiazepines, antipsychotics, diabetes drugs, and opioids. But what about antidepressants? Anticoagulants? Blood pressure meds? There’s no clear roadmap for 80% of the medications older adults take. A 2024 analysis of 3,569 clinical guidelines found only 7% mentioned deprescribing. Meanwhile, 93% focused on when to start a drug-not when to stop.
How to Start Deprescribing-Even If You’re Not a Doctor
You don’t need to be a clinician to make a difference. Here’s what you can do:- Ask for a med review-Every year, ask your doctor or pharmacist: “Is every medication I’m taking still necessary?”
- Bring all your pills-Not a list. The actual bottles. Pills get mixed up. Doses change. You’d be surprised how often the chart is wrong.
- Ask about tapering-Never stop cold turkey. Ask: “Can this be reduced slowly?”
- Track symptoms-Keep a simple log: “On Day 5 of lowering my pill, I felt calmer.” Or: “I had trouble sleeping after stopping X.”
- Use free tools-Go to deprescribing.org. Download the algorithms. Print them. Bring them to your appointment.
The Future: Deprescribing as Standard Care
Change is coming. Slowly, but surely. In June 2024, the American Medical Association issued its first official policy: doctors should routinely assess whether every medication is still needed. That’s huge. By 2026, Medicare will start measuring how often doctors deprescribe. Hospitals and clinics will be rated on it. That means money will follow. The FDA has funded over $8 million in deprescribing research since 2020. The EU has made it a priority. Canada has national guidelines. Australia? We’re behind, but catching up. AI tools are being developed to scan EHRs and flag high-risk combinations. Imagine your doctor’s system saying: “Patient on 8 medications. Three are high-risk for falls. Consider tapering X, Y, Z.” By 2030, experts predict deprescribing checks will be as routine as checking blood pressure.Final Thought: Less Is More
Medicine isn’t about stacking more pills on top of more pills. It’s about helping people live better-with fewer side effects, fewer trips to the ER, and more clarity in their days. Deprescribing isn’t giving up. It’s choosing quality over quantity. It’s listening to the patient, not the protocol. It’s having the courage to say: “You don’t need this anymore.” And sometimes, that’s the most powerful prescription of all.Is deprescribing safe for older adults?
Yes, when done properly. Multiple studies, including a 2023 JAMA Internal Medicine trial with 372 older adults, show that structured deprescribing reduces medication burden without increasing hospitalizations or adverse events. In fact, the rate of side effects stayed nearly the same between patients who stopped medications and those who didn’t. The key is tapering slowly, monitoring symptoms, and involving a pharmacist or trained clinician.
What medications are most commonly deprescribed?
The five most common classes with evidence-based deprescribing guidelines are: proton-pump inhibitors (PPIs), benzodiazepines and related sleep aids (BZRAs), antipsychotics (especially for dementia), antihyperglycemics (like insulin or sulfonylureas in older adults with stable glucose), and opioid analgesics. These are the drugs most likely to cause harm over time without clear benefit, especially in people over 65.
Can I stop my medication on my own?
No. Some medications, like benzodiazepines, antidepressants, or blood pressure drugs, can cause serious withdrawal symptoms if stopped suddenly. Always work with your doctor or pharmacist to create a safe tapering plan. Even if you feel fine, stopping abruptly can lead to rebound symptoms, increased anxiety, seizures, or dangerous blood pressure spikes.
How long does it take to deprescribe a medication?
It varies. For PPIs, tapering usually takes 4 to 8 weeks. Benzodiazepines may take 3 to 6 months, depending on dose and duration of use. Antidepressants often require 6 to 12 weeks of gradual reduction. The goal isn’t speed-it’s safety. Slower tapers reduce withdrawal risk and give time to monitor how the body responds.
What if I’m worried about symptoms coming back?
That’s normal. Many patients fear that stopping a medication will bring back old symptoms. The key is to set clear goals before starting: “If I feel less confused and can walk without falling, is that worth giving up this pill?” Work with your provider to track symptoms during tapering. Most people find that symptoms don’t return-or return much milder. If they do, you can always restart at a lower dose.
Are there tools I can use to help with deprescribing?
Yes. Deprescribing.org offers free, evidence-based algorithms for PPIs, benzodiazepines, antipsychotics, antihyperglycemics, and opioids. The STOPP/START criteria (version 3, 2021) and the American Geriatrics Society’s Beers Criteria (2023) are also widely used. Print them out and bring them to your appointment. They help guide the conversation and show your provider you’re informed.




12 Comments
David Barry-11 November 2025
Let’s be real - most GPs don’t have the bandwidth to do this right. I’ve seen patients on 10+ meds because no one ever asked if they still needed them. The Shed-MEDS framework? Solid. But it needs to be baked into EHRs, not left to the mercy of overworked docs. Pharma reps don’t show up to talk about stopping meds. They show up to push the next script. Systemic failure, not patient negligence.
Alyssa Lopez-12 November 2025
WTF is this woke med bullshit? You want to stop meds? Fine. But dont tell me we shouldnt treat hypertension or diabetes just bc someone’s old. These pills keep people ALIVE. You think grandma’s gonna survive without her blood pressure med? Nah. She’s gonna end up in the ER. This deprescribing crap is just another way for lefty docs to cut corners. And dont get me started on pharmacists runnin the show - they dont even have MDs!
Alex Ramos-12 November 2025
Biggest win I’ve seen? My aunt cut her PPI after 12 years. Went from foggy, dizzy, and falling to clear-headed and walking the dog daily. Tapered over 6 weeks with her pharmacist. No rebound heartburn. No disasters. Just… life. 🙌 deprescribing.org is a game-changer. Print the algorithms. Bring ‘em to your doc. They’re not gonna do it for you. You gotta lead.
edgar popa-14 November 2025
my grandma stopped her benzo and now she sleeps better without it. who knew? lol. maybe we dont need to be drugged up just bc we old. small wins matter.
Eve Miller-15 November 2025
It is profoundly irresponsible to suggest that patients can initiate deprescribing without clinical supervision. The notion that a layperson can interpret STOPP/START criteria or safely taper benzodiazepines without monitoring is not merely misguided - it is dangerous. The American Geriatrics Society Beers Criteria exists for a reason: to prevent harm. Dismissing pharmacological complexity as "inertia" is an affront to medical science.
Chrisna Bronkhorst-15 November 2025
PPIs are overprescribed 90 of the time but nobody talks about how the industry makes billions off them. Same with benzos. Pharma writes the guidelines. Docs follow the money. You think this is about health? Nah. It's about profit. And now they want you to trust the pharmacist? Same system. Same players.
Amie Wilde-17 November 2025
My mom’s on 7 meds. We brought all the bottles to her PCP last year. Turned out she was taking two different versions of the same blood pressure pill. She’s down to 4 now. Felt better in a week. Just ask. Bring the pills. Don’t assume anything.
Gary Hattis-18 November 2025
In South Africa, we don’t even have access to half the meds these folks are talking about. But the idea? Universal. My uncle in Johannesburg stopped his statin after a year - no heart issues, no side effects. He’s 78. Still tending his garden. The point isn’t just stopping pills. It’s asking: what’s the goal? To live longer? Or to live better? We forget that in the West. We’re obsessed with quantity over quality.
Esperanza Decor-19 November 2025
I’ve been researching this for months since my dad had a bad reaction to his antipsychotic. I didn’t know antipsychotics were used for dementia agitation until I saw the stats. 20% increased stroke risk? That’s insane. I printed the deprescribing.org guide and handed it to his neurologist. He actually listened. We’re tapering now. It’s scary but also… kind of empowering? Like we’re taking back control. Not just waiting for the next prescription.
Deepa Lakshminarasimhan-20 November 2025
Deprescribing? Sounds like a psyop. Who really benefits? Big Pharma? The government? The EHR companies? They want you dependent on meds so they can track you, sell your data, and keep billing. Once you stop the pills, you’re harder to control. They don’t want you healthy. They want you compliant. Watch the FDA funding - it’s all PR. They’ll never let you stop meds for real. This is just a distraction.
Erica Cruz-20 November 2025
Oh look, another feel-good article about "cutting pills." Meanwhile, real doctors are drowning in patients who need these meds. The JAMA study? Tiny sample size. And let’s not pretend pharmacists are saints - they’re just the next layer of bureaucratic grease. This isn’t innovation. It’s virtue signaling wrapped in clinical jargon. Real medicine is hard. This? It’s lazy.
Johnson Abraham-22 November 2025
lol so now we’re supposed to trust some app or website to tell us what meds to stop? next they’ll tell us when to breathe. my grandpa’s on 8 pills. he’s 82. he’s fine. you think he’s gonna stop his heart med bc some guy in canada wrote a blog? nah. he’s gonna keep takin em. and he’ll live longer than you. 🤡