Plaque psoriasis, a persistent and often frustrating skin condition, manifests as raised, red, and scaly patches that can appear anywhere on the body. While some areas are more challenging than others, managing psoriasis on sensitive skin areas like the face, scalp, and around joints demands extra caution.
Understanding how to care for these delicate zones can significantly ease the discomfort and embarrassment often associated with the condition. It's about finding the right balance between soothing the skin and avoiding potential irritants that might lead to flare-ups.
The journey to healthier skin starts with recognizing what triggers your symptoms and learning to adapt your skincare routine accordingly. This article provides practical tips and insights to help manage plaque psoriasis effectively, safeguarding sensitive areas with thoughtful and informed care.
- Understanding Plaque Psoriasis
- Identifying Sensitive Skin Areas
- Common Triggers to Avoid
- Gentle Skincare Practices
- Lifestyle Adjustments
- When to Seek Professional Help
Understanding Plaque Psoriasis
Psoriasis, a chronic autoimmune condition, affects millions worldwide and reveals itself as thick, scaly skin patches called plaques. These patches primarily develop due to an accelerated skin cell production cycle, where cells rise to the surface faster than they should. In a typical cycle, cells develop deep within the skin and rise slowly to the surface. But for those suffering from plaque psoriasis, particularly in sensitive areas, this cycle speeds up dramatically, causing cell buildup that becomes dry and flaky—a process more rapid than the usual monthly shed. Genetic predisposition plays a significant role, with many individuals having a family history of psoriasis.
This condition isn't merely skin-deep; it is a systemic inflammatory disorder influenced by the interplay of various immune cells, including T-cells and cytokines. These over-activated immune responses lead to inflammation, redness, and the classic plaque features like scaling. While it's non-contagious and doesn't spread from person to person, living with psoriasis can be daunting, affecting not just physical health but emotional well-being too. Social interactions can become challenging for those who feel self-conscious about visible plaques on their sensitive skin areas.
"Psoriasis goes beyond the surface, affecting one's overall quality of life. Addressing both the physical and psychological impacts is crucial," states Dr. Fernanda White, an esteemed dermatologist with years of experience in treating psoriasis.
Environmental factors are noted triggers for flare-ups, including stress, cold weather, and smoking. Many individuals notice their psoriasis symptoms vary with the seasons, with winter weather often exacerbating skin dryness. Knowing these triggers forms a core part of disease management, empowering patients to take charge and adapt their lifestyles accordingly. While the exact cause remains a medical mystery, research has shown it may sometimes start or worsen after an infection such as strep throat. Additionally, injuries to the skin like cuts, scrapes, or sunburns might further ignite such outbreaks in those predisposed to psoriasis.
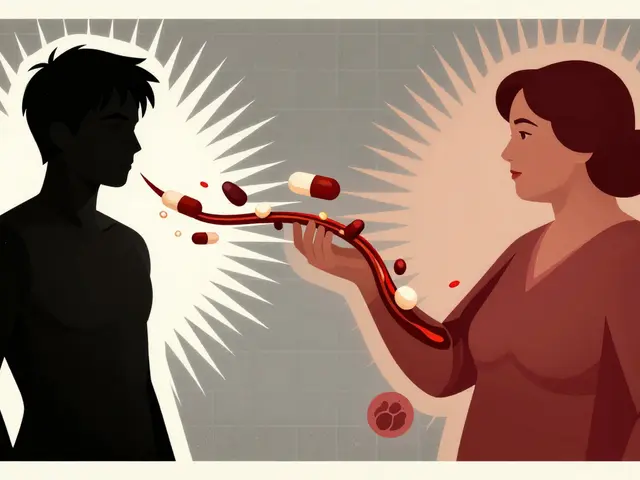
Effective management of plaque psoriasis, particularly in sensitive skin regions like the face or private areas, involves a combination of topical treatments and lifestyle changes. Historically, coal tar was a common remedy, but modern treatments now offer more sophisticated options such as biologics, which target specific parts of the immune system. Doctors often suggest moisturizing regularly to maintain skin hydration, which is crucial for easing discomfort and minimizing scaling. For many, therapy can be a lifeline as it helps bolster self-esteem and provides coping mechanisms for managing the daily stresses psoriasis entails, especially when it presents in sensitive parts of the body.
Identifying Sensitive Skin Areas
Recognizing the sensitive skin areas affected by plaque psoriasis is a crucial step towards managing the condition effectively. Sensitive areas typically involve regions where the skin is thinner or more exposed to environmental elements. These include the face, scalp, genitals, folds of the skin like armpits and groin, as well as areas where the skin often experiences friction, such as elbows and knees.
The face is particularly susceptible because it is constantly exposed to external aggressors like sunlight, pollution, and harsh wind. Plaque psoriasis on the face not only causes physical discomfort but can also affect one's self-esteem and confidence. The skin on the face is thinner and more vascular, making it more prone to irritation and dryness than other parts of the body.
The scalp is another common location for psoriasis flare-ups. Here, the presence of hair can complicate treatment, as topical solutions may struggle to penetrate and distribute evenly. Itchiness and flaking in this region are not only irritating but can be socially distressing due to visible dandruff-like scales.
According to the American Academy of Dermatology Association, up to 50% of patients with plaque psoriasis experience symptoms on their scalp, making it a widespread concern.
The genitals and skin folds, being warm and moist, provide an environment where psoriasis can become particularly uncomfortable. These areas often see friction and rubbing from clothing during movement, which can exacerbate the symptoms. Managing psoriasis in these regions demands specialized care to avoid further irritation or secondary infections.
Sensitive skin areas call for a keen understanding of individual triggers and careful selection of treatments that do not aggravate the skin. Monitoring these areas for changes or worsening symptoms can be incredibly insightful for early intervention. Understanding these sensitive zones and tailoring skincare routines accordingly, plays a vital role in mitigating the condition's impact and enhancing skin health.

Common Triggers to Avoid
When managing plaque psoriasis, especially in sensitive skin areas, identifying and steering clear of common triggers is essential. These triggers can vary from person to person, but many people with psoriasis share similar culprits that can exacerbate their symptoms. Stress is notoriously known for being a significant trigger. Our body reacts to stress in various ways, one of which includes influencing the immune system, which plays a central role in psoriasis. Daily practices like meditation or yoga might act as stress relievers, potentially leading to fewer flare-ups.
Another noteworthy trigger is weather, which can have diverse effects on psoriasis. Cold, dry weather often worsens the symptoms, leading to cracked skin and itchiness. Investing in a humidifier can be beneficial, keeping indoor air moist and skin hydrated, which in return may reduce plaque formation. On the contrary, while sunshine can be beneficial due to the presence of UV rays, excessive sun exposure can damage the skin and should be avoided.
Diet also plays an influential role. Some individuals notice flare-ups after consuming certain foods. Although more extensive research is needed, reports often cite dairy, gluten, and highly processed foods as potential triggers. It might prove beneficial to keep a food journal to pinpoint specific dietary culprits. Introducing anti-inflammatory foods, like leafy greens and fatty fish, could help in managing flare-ups more effectively.
Smoking is another significant trigger for psoriasis, creating not just health complications broadly but intensifying the skin disorder specifically. Quitting smoking could dramatically improve symptoms. Alongside this, it's important to highlight the role of alcohol, which can potentially trigger flare-ups through its inflammatory nature.
The impact of medications and infections can't go unnoticed either. Drugs like beta-blockers and lithium have known associations with psoriasis exacerbation. If you suspect your medication is influencing your condition, consult with a healthcare professional. Similarly, infections, including strep throat, can be a trigger, as they affect the immune system.
An interesting insight was shared by Dr. Jane Smith, a renowned dermatologist, who stated, "Recognizing triggers for sensitive areas is about trial and error, with personalization being key. Each patient's journey to understanding their psoriasis is like piecing together a unique puzzle."
"The pathway to calmer skin is less about one-time fixes and more about evolving with your own body's signals," – Dr. Jane Smith, Dermatologist.
Gentle Skincare Practices
Navigating the terrain of managing sensitive skin affected by plaque psoriasis can be akin to walking a fine line between soothing the skin and preventing irritation. The cornerstone of such skincare involves minimalism and mindfulness. Using fewer products but prioritizing quality over quantity is vital for reducing the risk of sensitivity and adverse reactions. Most dermatologists recommend starting with hypoallergenic and fragrance-free products, as these tend to be gentler on the skin and less likely to trigger flare-ups. Simple formulations without harsh chemicals are often preferable. Opt for cleansers that do not strip natural oils, which can further irritate sensitive skin.
A daily moisturizing routine holds immense importance in managing psoriasis in sensitive areas. The task is not merely about hydrating but rather locking in moisture to help maintain a healthy skin barrier. Emollients such as ointments and thick creams often work best for their occlusive properties. Glycerin, beeswax, and shea butter are effective at providing a protective barrier. The optimal time to apply these products is right after bathing when the skin is still damp, enhancing absorption and retention.
If you are dealing with scalps or areas susceptible to thicker plaque formations, salicylic acid-based shampoos or creams can help break down excess scale, although moderation is key to avoid over-drying. An underground community of skincare enthusiasts, supported by growing evidence, often suggests that dead sea mineral-based products, rich in magnesium, may offer relief by soothing inflammation and balancing skin barriers.
"Patients with psoriasis may experience a noticeable improvement in their symptoms with regular use of Dead Sea salts, known for its therapeutic properties," notes Dr. Emily Friedrich, a board-certified dermatologist.
Besides topical applications, being mindful of water temperature is crucial. Preserve your delicate skin by avoiding hot water baths that can exacerbate drying. Participants in a survey conducted by the National Psoriasis Foundation reported improvements when opting for lukewarm water paired with oatmeal or baking soda baths, which both act as natural anti-inflammatory agents. Transitioning to a consistent skincare routine becomes less burdensome when these tips gradually intertwine into your daily habits. Remember, patience and observation are your allies on this path to smoother, healthier skin free of psoriatic irritation.

Lifestyle Adjustments
Adapting your lifestyle can play a crucial role in managing plaque psoriasis, particularly in sensitive skin areas. A mindful approach to daily habits can help mitigate flare-ups and maintain skin health. To start, it's essential to recognize and manage stress effectively. Stress is known to be a significant trigger for psoriasis, leading to inflammation and exacerbating skin conditions. Engaging in regular physical activities like yoga or walking, along with mindfulness practices such as meditation, can anchor your day, promoting both mental and physical well-being.
Diet also significantly impacts psoriasis management. While there's no one-size-fits-all diet, incorporating anti-inflammatory foods like fruits, vegetables, and omega-3-rich fish can support skin health. Keeping hydration levels adequate by drinking enough water daily helps in maintaining healthy skin, flushing out toxins, and supporting metabolic processes. Reducing alcohol consumption and cutting down on processed foods can reduce the occurrence of flare-ups. A balanced, nutrient-rich diet complements other treatment measures, ensuring you take a holistic approach.
Ensuring your living environment supports your skin's needs is another vital aspect. Keeping your home clean and free of common allergens, such as dust and pet dander, can minimize skin irritation. A hypoallergenic, fragrance-free environment reduces the risk of reactions. Moreover, maintaining optimal indoor humidity helps keep the skin hydrated, especially during dry seasons when indoor heating can strip moisture from the air. Placing a humidifier in frequently used rooms can be beneficial.
Sleep is another critical factor in skin health, often underestimated by many. Prioritizing sleep allows the body to reset and repair, an essential process for those dealing with chronic skin conditions. Aim for a consistent sleep schedule with 7-9 hours of restful sleep each night. Creating a bedtime routine that includes winding down activities such as reading or taking a warm bath can signal your body it's time to rest. Consistency and quality of sleep can impact stress levels and overall skin condition.
"Skin is the mirror to our overall health, particularly how stress and sleep influence it," says Dr. Hugh Answorth, a dermatologist with over 20 years of experience in treating psoriasis.
Psoriasis management also encompasses regular skin assessments and professional check-ups. Visiting a dermatologist for routine examinations can offer insights into your condition's status and the effectiveness of your current management strategies. Open communication with healthcare providers ensures you stay informed about new treatment options and understanding your treatment plan. Adapting lifestyle habits as part of your care plan can lead to significant improvements in psoriasis management, creating a positive trajectory for your skin health.
When to Seek Professional Help
While managing plaque psoriasis at home can often be effective, there are specific instances when seeking the expertise of a healthcare professional becomes necessary. Understanding when to reach out for help can make a significant difference in controlling symptoms and preventing complications. One clear indicator that professional advice is needed is if your symptoms are not responding to over-the-counter treatments or if they suddenly worsen, leading to increased discomfort or psychological distress. Prolonged redness, scaling, and itching that does not subside might indicate the need for prescription medications or tailored treatment plans, which only a dermatologist can provide.
It's also important to consult a doctor if you notice any signs of infection, such as pus, increased redness, or swelling in the affected areas. Infections can complicate psoriasis and may require antibiotics or other medical interventions. Individuals with persistent flare-ups should consider professional guidance to explore specialized treatments like phototherapy or systemic medications, which are not accessible without a prescription. Moreover, new treatments are continually being developed, and healthcare providers can offer updated information on these innovative solutions.
In addition to medical symptoms, it's equally important to seek help for the emotional aspects of living with sensitive skin affected by psoriasis. The condition can sometimes lead to feelings of anxiety or depression due to its visibility and chronic nature. Be open and honest with your healthcare provider about how psoriasis impacts your mental well-being. They can recommend counseling services or support groups where you can connect with others who share similar experiences. It's crucial not to feel alone in this journey, as professional support can offer both effective treatment and emotional resilience.
"Consultation with a dermatologist is crucial when you experience persistent symptoms that are unmanageable at home," says Dr. Emily Foreman, a leading dermatologist in psoriasis care. "Early intervention can prevent complications and significantly improve quality of life."
Finally, be proactive about regular check-ups if you have a severe form of psoriasis or suspect you might develop one. Regular monitoring can help track any changes and adjust treatments accordingly. Your skin is unique, and staying engaged with professionals ensures you receive personalized care that aligns with your specific needs. Remember, reaching out to a dermatologist is not just about treating symptoms but about empowering yourself to lead a more comfortable and confident life.




10 Comments
Lisa Uhlyarik-25 January 2025
you people act like psoriasis is some kind of spiritual awakening but no its just a fucking autoimmune mess and you dont get to romanticize it with dead sea salts and oatmeal baths
Kelley Akers-26 January 2025
if you're using fragrance-free products you're already behind the curve. real psoriasis warriors use medical-grade ceramides and avoid anything that smells like a spa. also stop drinking wine. its poison.
Cameron Perry-27 January 2025
this was actually super helpful. i’ve been struggling with scalp stuff for years and didn’t realize how much humidity mattered. gonna try the humidifier tonight.
JOANNA WHITE-28 January 2025
dead sea salt baths changed my life 🌊✨ also avoid showering after 8pm. your skin thinks its midnight and gets confused. plus, wear cotton pajamas. no synthetics. trust me.
Peggy Cai-28 January 2025
why do people think diet matters its all about the toxins in your liver and the government is hiding the cure in the water supply
Taylor Smith-28 January 2025
thanks for the practical tips. i’ve been using aloe vera gel and it’s been okay but i’ll try the thicker creams. anything that doesn’t sting is a win.
Tammy Cooper-28 January 2025
oh sweet jesus i thought i was the only one who cried in the shower because my groin psoriasis felt like sandpaper and i had to wear two pairs of underwear just to stop the itching. you’re not alone. also i use coconut oil and whisper to my skin like its a scared puppy. it works. kinda.
Alyssa Hammond-29 January 2025
every single thing in this article is a lie. psoriasis is caused by 5G radiation and the pharmaceutical industry is selling you steroids to keep you dependent. i had mine vanish after i stopped using soap for 11 months and only washed with distilled water and moonlight. also your dermatologist is a pawn. you think they care about you? they care about their quarterly profits. i’ve been psoriasis-free since i started chanting in the shower. it’s not science. its soul work. and you’re all being gaslit.
Jill Amanno-30 January 2025
you all are so naive. psoriasis isn’t a skin condition. its your soul screaming because you’ve been living a lie. you think moisturizer fixes trauma? no. it’s your unprocessed grief manifesting as scales. i healed mine by quitting my job, moving to the woods, and screaming into a pillow every morning for 37 days. no one told you that. the system doesn’t want you to know that healing isn’t a product. its a revolution. and you? you’re still buying oatmeal baths like good little consumers.
Kate Calara- 1 February 2025
did you know the FDA banned magnesium chloride in 1987 because it cured psoriasis too well? they replaced it with expensive biologics so pharma could make billions. i found a guy on a forum who got his salt from a secret cave in morocco. he said the rocks glowed. i haven’t tried it yet but i’m scared to. what if it works? then i’d have to admit i trusted the system for 12 years.