One glass of grapefruit juice in the morning might seem like a healthy habit-until it turns into a silent danger if you’re on certain medications. This isn’t just a myth or old wives’ tale. It’s a well-documented, potentially life-threatening interaction that affects more than 85 medications, including common ones like statins, blood pressure pills, and anti-anxiety drugs. And the worst part? Many people have no idea they’re at risk.
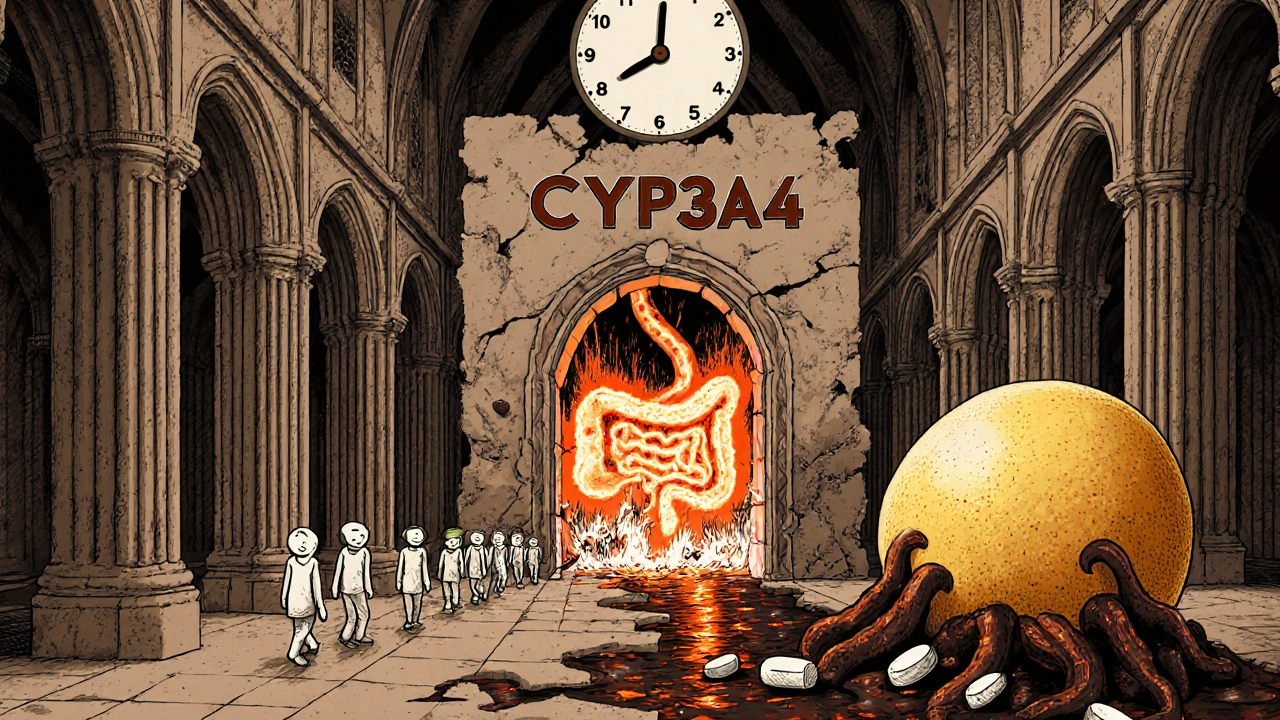
How Grapefruit Juice Changes How Your Body Handles Medicine
Grapefruit juice doesn’t just taste tangy-it changes how your body absorbs and breaks down drugs. The culprits are chemicals called furanocoumarins, mainly bergamottin and 6’,7’-dihydroxybergamottin. These aren’t found in oranges or tangerines. They’re unique to grapefruit and a few close relatives like Seville oranges and pomelos.
When you drink grapefruit juice, these compounds attack enzymes in your small intestine called CYP3A4. These enzymes normally break down a large portion of medications before they even enter your bloodstream. Think of them as gatekeepers. When they’re shut down by grapefruit, more of the drug slips through untouched. That means your body ends up with way more of the medicine than intended-sometimes up to eight times more.
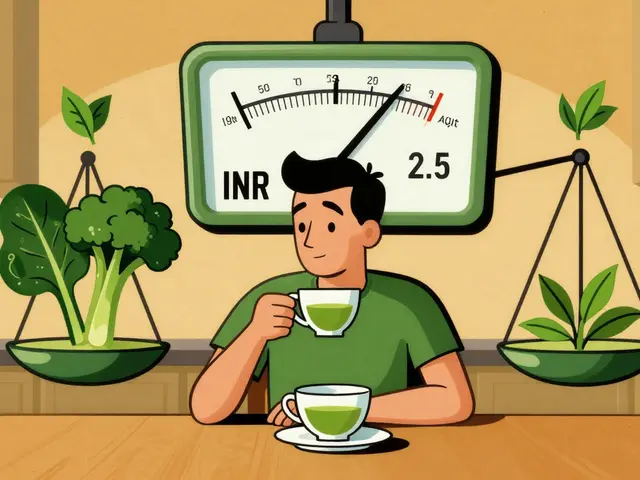
It’s not just about absorption. Grapefruit juice also blocks OATP transporters, which help move some drugs into your cells. For medications like fexofenadine (Allegra), this means less of the drug gets absorbed, making it less effective. So grapefruit can either boost or weaken a drug, depending on how it’s processed.
Which Medications Are Most at Risk?
Not all drugs are affected equally. The real danger lies in those that are heavily processed by CYP3A4 and have a narrow safety window-meaning even a small increase in blood levels can cause serious side effects.
Statins are one of the most common culprits. Simvastatin and lovastatin, used to lower cholesterol, can cause severe muscle damage (rhabdomyolysis) when combined with grapefruit juice. A single 200mL glass can raise simvastatin levels by 330%. Atorvastatin (Lipitor) also carries risk, though less so. But pravastatin, rosuvastatin, and fluvastatin? Safe. They don’t rely on CYP3A4.
Calcium channel blockers like felodipine and nifedipine, used for high blood pressure, can drop your blood pressure too far, causing dizziness, fainting, or even heart issues. Felodipine levels can spike by 300% to 800% with grapefruit juice. Amlodipine, however, is unaffected.
Benzodiazepines like midazolam and triazolam-used for anxiety and sleep-can make you excessively drowsy or even cause breathing problems. Midazolam’s blood levels can jump 515%.
Immunosuppressants like cyclosporine and tacrolimus, taken after organ transplants, become dangerously toxic. Even small increases can damage the kidneys or liver.
Antiarrhythmics like amiodarone can trigger irregular heart rhythms. Antidepressants like sertraline and buspirone may cause serotonin syndrome-fever, confusion, rapid heartbeat.
And then there are the surprises. Theophylline (for asthma) and itraconazole (an antifungal) actually become *less* effective with grapefruit juice. Why? The mechanism isn’t fully understood, but it’s another reason not to assume you’re safe just because a drug isn’t on the “high-risk” list.
How Much Juice Is Too Much?
You don’t need a whole pitcher. As little as 200mL-about 6.8 fluid ounces, or a single glass-can trigger an interaction. It doesn’t matter if it’s fresh-squeezed, from concentrate, or from the whole fruit. The furanocoumarins are in all forms. White grapefruit has slightly more than pink, but both are dangerous.
And the effect lasts. Once the enzymes are blocked, your body needs about 72 hours to make new ones. So even if you drink grapefruit juice at breakfast and take your medication at night, you’re still at risk. The interaction isn’t about timing-it’s about whether the enzyme is active when the drug passes through your gut.
Who’s Most at Risk?
Older adults are especially vulnerable. About 42% of people over 65 take five or more medications. Many of those are on statins, blood pressure drugs, or heart medications-all of which can interact with grapefruit. The American Geriatrics Society lists grapefruit interactions as a potentially inappropriate practice for older patients.
People with liver or kidney disease are also at higher risk because their bodies clear drugs more slowly. And genetic differences play a role. Some people naturally have more CYP3A4 enzymes in their gut, making them more sensitive to grapefruit’s effects. A 2023 study found that a specific gene variant (CYP3A4*22) makes interactions even stronger.
Yet, studies show only 28% of patients can correctly identify which of their medications are affected-even after being told. And 47% of patients on high-risk drugs still consume grapefruit juice despite warnings. Among those over 65, non-compliance hits 63%.
What About Other Citrus Fruits?
Regular oranges, tangerines, and clementines are safe. They don’t contain furanocoumarins. But Seville oranges (used in marmalade) and pomelos? Avoid them. They have the same chemicals as grapefruit. Some hybrid citrus fruits may too-so when in doubt, check the label or ask your pharmacist.
What Should You Do?
If you take any prescription medication, ask your pharmacist: “Is it safe to drink grapefruit juice with this?” Don’t assume it’s fine. Even if your doctor didn’t mention it, they may not have thought to ask.
Check your medication labels. The FDA now requires grapefruit interaction warnings on 21 high-risk drugs, including simvastatin, felodipine, and cyclosporine. If your label says “avoid grapefruit,” take it seriously.
If you’re on a high-risk drug, switch to a safer alternative. Many statins, blood pressure meds, and anxiety medications have versions that don’t interact. Your doctor can often switch you without losing effectiveness.
And if you love the taste? Try alternatives like orange juice, apple juice, or water. No need to give up your morning routine-just make it safe.
Why Is This Still a Problem?
Despite decades of research, awareness is shockingly low. Only 37% of pharmacists consistently warn patients about grapefruit interactions. Many patients assume “natural” means “safe.” Others think one glass won’t hurt. But this isn’t about occasional indulgence-it’s about cumulative risk.
The European Medicines Agency reports 85 serious adverse events and 12 deaths linked to grapefruit interactions in the EU between 2000 and 2019. In the U.S., it’s estimated that 42% of adults over 40 take at least one medication affected by grapefruit juice.
Pharmaceutical companies are responding. Extended-release versions of some drugs (like felodipine) reduce interaction severity. Drug interaction software now flags grapefruit in 18% of all food-drug alerts. Electronic health records include 128 specific grapefruit warnings.
But the best solution remains simple: avoid it. Until you know for sure your meds are safe, skip the grapefruit. The science is clear. The risks are real. And the consequences can be irreversible.
What’s Next?
Researchers are exploring ways to genetically modify grapefruit to remove furanocoumarins-early trials are underway. Some scientists are even looking at whether the interaction mechanism could be harnessed to improve drug delivery for certain therapies.
But for now, the message hasn’t changed: if your medication is on the list, don’t risk it. One glass of juice isn’t worth a hospital stay. Or worse.
Can I drink grapefruit juice if I take a low dose of my medication?
No. Even small doses of affected medications can become dangerous with grapefruit juice. The interaction isn’t about the dose of the drug-it’s about how much of it enters your bloodstream. Grapefruit juice can push even a low dose into toxic levels. There’s no safe amount if your medication is on the high-risk list.
How long should I wait after drinking grapefruit juice before taking my medicine?
You can’t just wait a few hours. Grapefruit juice causes irreversible damage to intestinal enzymes, and it takes about 72 hours (three days) for your body to replace them. So even if you drink grapefruit juice at breakfast and take your pill at night, you’re still at risk. The only safe option is to avoid grapefruit entirely while on the medication.
Are all types of grapefruit equally dangerous?
Yes. Whether it’s white, pink, or red, all grapefruit contain the same harmful compounds-furanocoumarins. White grapefruit may have slightly higher levels, but pink and red are still dangerous. Fresh fruit, juice, frozen concentrate, and even grapefruit-flavored products can trigger interactions. Avoid them all.
What if I’ve been drinking grapefruit juice for years with no problems?
That doesn’t mean you’re safe. Individual responses vary widely-some people naturally have more CYP3A4 enzymes, so grapefruit affects them more. You might have been lucky so far, but your body changes over time. Age, liver health, and other medications can all shift your risk. What was fine last year might be dangerous today.
Can I switch to a different medication to avoid this problem?
Yes, often you can. For example, if you’re on simvastatin, your doctor can switch you to pravastatin, rosuvastatin, or fluvastatin-all of which are not affected by grapefruit. The same applies to blood pressure medications like felodipine versus amlodipine. Always ask your doctor or pharmacist: is there a safer alternative? Many options exist.
Is orange juice a safe substitute?
Yes, regular orange juice, tangerines, and clementines are safe. They don’t contain furanocoumarins. But avoid Seville oranges (used in marmalade) and pomelos-they’re just as dangerous as grapefruit. Always check the label if you’re unsure.
Why don’t all doctors warn patients about this?
Many doctors assume patients will read the label or hear it from the pharmacist. But studies show only 37% of pharmacists consistently counsel patients, and only 28% of patients remember which meds are affected. It’s a gap in communication. Don’t wait for your doctor to bring it up-ask directly. Your safety depends on it.




8 Comments
Diane Tomaszewski-16 November 2025
Grapefruit juice messes with your meds and nobody tells you until it's too late
Teresa Smith-17 November 2025
It's not just about grapefruit-it's about how our healthcare system fails to communicate basic risks. We're told to eat healthy, but no one warns us that a single glass of juice can turn a life-saving drug into a poison. The burden shouldn't be on patients to memorize food-drug interactions. Pharmacies should print warnings on prescriptions. Doctors should have mandatory alerts in their EHRs. This isn't just medical knowledge-it's public safety. And yet, we treat it like a footnote.
Dan Angles-19 November 2025
While the scientific basis for grapefruit-drug interactions is well-established, the persistence of this issue underscores a systemic failure in patient education. The pharmacokinetic mechanisms involving CYP3A4 inhibition and OATP transporter blockade are complex, yet the clinical implications are unequivocal. Patients on narrow-therapeutic-index medications-particularly statins, calcium channel blockers, and immunosuppressants-must be counseled with unambiguous directives. The 72-hour enzyme recovery window further necessitates complete abstinence, not temporal separation. This is not a matter of dietary preference but of pharmacological integrity.
David Rooksby-21 November 2025
Let me tell you something they don't want you to know-big pharma doesn't care if you die from grapefruit juice because they make more money off you in the ER. They design drugs to be broken down by CYP3A4 on purpose-it's called a 'metabolic trap' so you have to keep buying the same pills. And why? Because if they made a version that didn't interact, you'd switch to generics and they'd lose billions. That's why they only warn on 21 drugs out of 85+-they're cherry-picking the ones where lawsuits are unavoidable. Meanwhile, your pharmacist? They're paid by the drug companies to push the brand-name stuff. And don't get me started on how the FDA gets their funding from industry lobbyists. This isn't science-it's a profit scheme disguised as medicine. I've seen the internal memos. You think your doctor doesn't know? They do. They just can't say it out loud. Wake up.
Melanie Taylor-21 November 2025
OMG I just realized I’ve been drinking grapefruit juice with my blood pressure med for 3 years 😱 I’m so glad I read this!! I’m switching to orange juice now!! 🍊❤️ Thanks for sharing this life-saving info!! I’m telling everyone!! 💪 #GrapefruitWarning #MedSafety #HealthIsWealth
ZAK SCHADER-23 November 2025
Yall actin like grapefruit is the devil but if you actually knew how to read a label you wouldn't be this dumb. Also why are we letting foreigners tell us what to eat? This is why america is falling apart. My grandpa took grapefruit with his pills for 50 years and he lived to 92. Stop fearmongering. #AmericaFirst #StopTheHysteria
Danish dan iwan Adventure-25 November 2025
CYP3A4 inhibition is dose-independent and irreversible. Furanocoumarins bind covalently to the enzyme's active site, inducing proteasomal degradation. No threshold exists. Patient non-compliance correlates with socioeconomic status and health literacy deficits. Mitigation requires structured pharmacist-led interventions. Evidence-based guidelines are clear. Implementation remains poor.
Ankit Right-hand for this but 2 qty HK 21-25 November 2025
Everyone’s panicking over grapefruit juice like it’s a pandemic. Meanwhile, 80% of Americans are on 3+ meds and still drinking coffee, smoking, eating sugar, and taking OTC painkillers like they’re candy. You think one fruit is the real threat? You’re missing the forest for the citrus. This is a distraction tactic by the medical-industrial complex to make you feel like you’re in control when you’re not. Your real danger? Polypharmacy. Your real enemy? The system that sells you 12 pills a day and calls it healthcare. Grapefruit? Just the scapegoat.