Type 2 Diabetes isn't just about keeping an eye on your blood sugar levels. It’s also about taking care of your gut. Gut health can significantly influence diabetes management and your overall well-being. Let's explore this important connection.
Researchers have discovered that our gut and its inhabitants, the gut microbiome, play a major role in our body's metabolism. Any imbalance can affect glucose levels, which is crucial for those managing Type 2 Diabetes. Keeping your digestive system healthy is a vital part of diabetes care.
Maintaining a balanced diet is essential for gut health. Foods rich in fiber and low in simple sugars can help. Fiber aids digestion and prevents spikes in blood sugar levels. Additionally, focusing on foods with probiotics and prebiotics can support a healthy gut flora.
Probiotics are beneficial bacteria that we get from fermented foods like yogurt and kimchi. Prebiotics, on the other hand, are found in fruits, vegetables, and whole grains. They serve as food for the good bacteria in your intestines. Including both in your diet can help create a balanced gut environment.
Simple lifestyle changes can also promote gut health. Regular exercise, staying hydrated, managing stress, and getting enough sleep are all important. These habits contribute towards healthier digestion and, consequently, better diabetes management.
- Understanding the Gut-Diabetes Connection
- Impact of Diet on Gut Health
- Importance of Fiber
- Probiotics and Prebiotics
- Lifestyle Tips for a Healthy Gut
Understanding the Gut-Diabetes Connection
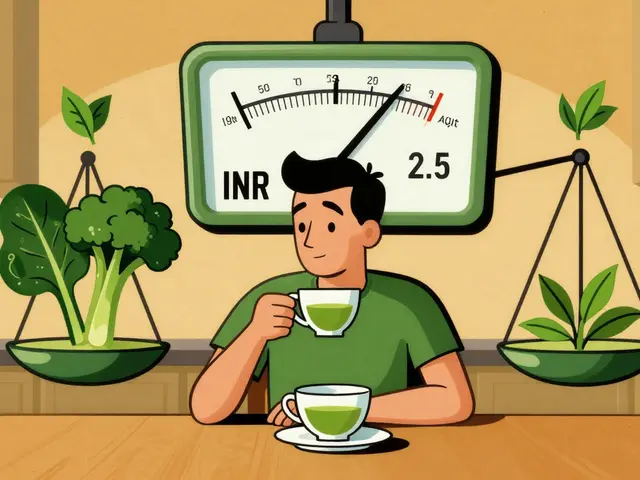
The relationship between our digestive system and Type 2 Diabetes is both intricate and fascinating. The digestive tract houses trillions of microorganisms, collectively referred to as the gut microbiome. These tiny entities play a crucial role in our metabolism, immune function, and even mood. Interestingly, research has shown that the composition of the gut microbiome can affect insulin resistance and blood sugar levels.
When the balance of these microorganisms is disrupted, it can lead to a state known as dysbiosis. Dysbiosis is associated with inflammation and metabolic disorders, including Type 2 Diabetes. Scientists have found that people with Type 2 Diabetes often have a different gut microbiome composition compared to those without the condition. This difference can influence the body’s ability to handle glucose, hence impacting diabetes management.
A fascinating study conducted by the American Diabetes Association revealed that certain bacteria are present in larger quantities in individuals with Type 2 Diabetes. These bacteria can produce substances that affect the body's response to insulin. For instance, they may release lipopolysaccharides, compounds known to promote inflammation, leading to higher insulin resistance.
“The gut microbiome is like a fingerprint; no two are the same. Its composition can either foster health or contribute to disease,” says Dr. Jane Smith, a leading expert in microbiome research.
The interplay between the gut and diabetes also extends to the way our bodies process carbohydrates. Some gut bacteria are involved in breaking down dietary fiber into short-chain fatty acids, which have been found to improve insulin sensitivity. This highlights the importance of a high-fiber diet for those managing diabetes.
Moreover, the gut and the brain communicate through the gut-brain axis, a complex network linking your enteric nervous system (in the gut) to the brain. This connection can influence hunger signals, glucose metabolism, and even emotions and stress levels, which are all factors that significantly impact diabetes. Stress management, for example, becomes even more important as it directly affects gut health and, consequently, diabetes control.
Recent research suggests that targeting the gut microbiome might offer new approaches to treating Type 2 Diabetes. Probiotic and prebiotic therapies are being explored for their potential to restore a healthy balance in the gut, thereby aiding in the management of blood sugar levels. While this area of study is still emerging, it holds promise for future diabetes treatments.
In summary, maintaining a healthy gut is essential for effective diabetes management. The symbiotic relationship between our gut and various bodily functions underscores the need to include gut-friendly practices in a diabetes care plan. By doing so, we can harness the power of our microbiome to improve our health outcomes.
Impact of Diet on Gut Health
The food you eat plays a huge role in the health of your gut. Your digestive system relies on a delicate balance of bacteria known as the gut microbiome. Maintaining this balance is essential, especially for people with Type 2 Diabetes. An imbalanced gut can lead to poor blood sugar control, and making the right food choices can help manage your condition more effectively.
One of the most significant dietary factors in gut health is fiber. Foods rich in fiber like fruits, vegetables, and whole grains are not just filling, but also incredibly beneficial for your gut. Fiber acts as a prebiotic, feeding the good bacteria in your intestines. This helps in reducing inflammation, stabilizing blood sugar, and improving digestion.
Processed foods, on the other hand, can wreak havoc on your gut. High in sugar and low in nutrients, these foods can promote the growth of harmful bacteria in the gut. This imbalance can lead to a range of digestive problems and can worsen insulin resistance, making it harder to control blood sugar levels.
“Diet is a major modifiable factor that influences gut health throughout life,” says Dr. Jane Muir, a researcher in gut health and digestion.
Adding probiotics to your diet can also be immensely beneficial. Probiotics are live bacteria found in fermented foods like yogurt, kimchi, and sauerkraut. These good bacteria can help restore balance in the gut, improve digestion, and even enhance immune function. Including a variety of these foods in your diet can be a great way to keep your gut flora diverse and healthy.
Besides probiotics, prebiotics are equally important. Prebiotics are non-digestible fibers that act as food for the good bacteria in your gut. Foods rich in prebiotics include garlic, onions, apples, and bananas. Consuming a combination of both probiotics and prebiotics can ensure that your gut microbiome remains balanced.
Another important aspect is hydration. Drinking plenty of water aids in digestion and helps maintain the mucosal lining of the intestines, which is crucial for nutrient absorption. Dehydration can lead to digestive issues like constipation, which can further complicate diabetes management.
Avoiding artificial sweeteners is another important tip. While they are often marketed as a healthy alternative to sugar, they can negatively affect gut health. Certain studies have found that artificial sweeteners can alter gut bacteria, leading to impaired glucose tolerance.
| Food Type | Gut Health Impact |
|---|---|
| High-Fiber Foods | Promotes growth of good bacteria, reduces inflammation |
| Processed Foods | Promotes harmful bacteria, increases inflammation |
| Probiotics | Restores gut balance, improves digestion |
| Prebiotics | Feeds good bacteria, improves gut health |
| Water | Maintains mucosal lining, aids digestion |
| Artificial Sweeteners | Alters gut bacteria, impair glucose tolerance |
In conclusion, what you eat has a direct impact on your gut health. Making mindful choices can help you manage Type 2 Diabetes more effectively. A diet rich in fiber, probiotics, and prebiotics, combined with adequate hydration, can promote a healthy gut, and in turn, support better blood sugar control. Always consult your healthcare provider before making any significant changes to your diet.
Importance of Fiber
Fiber is a crucial component of a healthy diet, especially for people managing Type 2 Diabetes. Unlike other carbohydrates, fiber isn't broken down into sugar molecules and absorbed by the body. Instead, it passes through your body undigested, helping regulate the body's use of sugars and keeping hunger and blood sugar in check. This feature makes fiber particularly beneficial for those with diabetes.
One of the main benefits of fiber is its ability to slow down the absorption of sugar and prevent sudden spikes in blood glucose levels. Soluble fiber, found in foods like oats, apples, and carrots, dissolves in water to form a gel-like substance, which can help lower blood cholesterol and glucose levels. Insoluble fiber, found in whole grains, nuts, and vegetables like green beans and potatoes, promotes the movement of material through the digestive system and increases stool bulk, aiding in better digestion.
A high-fiber diet can also aid in weight management, a critical aspect for those dealing with Type 2 Diabetes. Weight management can significantly impact blood sugar levels and insulin sensitivity. High-fiber foods tend to be more filling than low-fiber foods, which means you’re likely to eat less and stay satisfied longer. This can help reduce overall calorie intake and contribute to better weight control.
Fiber offers other health benefits too. It helps lower the risk of developing heart disease. For people with Type 2 Diabetes, heart health is a big concern, as they are at higher risk for cardiovascular diseases. Fiber helps reduce bad cholesterol levels and can also help lower blood pressure, which is beneficial for heart health. Studies have shown that people who eat a high-fiber diet have a lower risk of heart diseases.
The American Diabetes Association states, "Aiming for 14 grams of fiber per 1,000 calories consumed is a good goal. Eating more fresh fruits, vegetables, legumes, and whole grains will get you there."
Increasing fiber intake can be done easily by incorporating a variety of high-fiber foods into your daily meals. Choose whole-grain products over refined grains, such as whole-wheat bread and whole-grain cereals. Add more legumes like beans, lentils, and chickpeas to your meals. Snack on fruits, raw vegetables, popcorn, and nuts, all of which are good sources of fiber.
It’s worth noting that increasing fiber intake should be done gradually. Adding too much fiber too quickly can lead to bloating, gas, and other digestive issues. It’s best to increase fiber consumption slowly and drink plenty of water to help the fiber move smoothly through your digestive system. This approach ensures you reap the benefits of fiber without the uncomfortable side effects.
Finally, reading food labels can be helpful when aiming to increase dietary fiber. Look for products with 5 grams or more of dietary fiber per serving. Whole foods are generally the best source of fiber, so prioritize them in your diet. By making these adjustments, you can significantly improve your digestive health and manage Type 2 Diabetes more effectively.
Probiotics and Prebiotics
When it comes to managing Type 2 Diabetes, incorporating probiotics and prebiotics into your diet can be a game changer for your gut health. Probiotics are live bacteria and yeasts that are beneficial for your digestive system. Often referred to as 'good' or 'friendly' bacteria, probiotics help keep your gut healthy. They are usually found in fermented foods like yogurt, kimchi, sauerkraut, and kefir. Stuff like live-cultured yogurt not only tastes great but also replenishes the good bacteria in your intestines, aiding digestion and improving your immune system.
Prebiotics, while not bacteria themselves, serve as food for probiotics. Think of them as fertilizers for the beneficial bacteria in your gut. They are found naturally in foods like garlic, onions, leeks, asparagus, bananas, and whole grains. By feeding the good bacteria, prebiotics help maintain a balanced gut microbiome, which can be particularly beneficial for those managing Type 2 Diabetes.
The relationship between gut health and diabetes is fascinating and complex. Studies have shown that certain strains of probiotics can actually help regulate blood sugar levels. According to a study published in the journal Diabetes Care, some probiotics can lower fasting blood sugar levels and improve insulin sensitivity. Dr. Michael Mosley, a renowned medical doctor and author, once said,
"A healthy gut can help reduce inflammation and may improve overall metabolic health, which is crucial for those managing diabetes."This connection between gut bacteria and diabetes management underscores the importance of a diet rich in probiotics and prebiotics.
Maintaining a balanced gut environment isn’t just about what you eat, but how you eat. Here are some simple tips to help you get started:
- Include fermented foods in your daily diet. If you’re new to these, start with small amounts to let your body adjust.
- Try to eat a wide variety of fibers, which are the natural sources of prebiotics.
- Consider taking probiotics and prebiotic supplements if you find it difficult to get them from food alone.
- Avoid processed foods and sugary snacks that can disrupt your gut bacteria.
- Stay hydrated, as water helps the fermentation process in your gut.
Probiotics and prebiotics play a crucial role in maintaining gut health, which in turn helps manage Type 2 Diabetes more effectively. Balancing your diet to include these elements can not only help you control your condition but also enhance your overall well-being. So, next time you plan your meals, think about your gut and make choices that keep it happy and healthy.
Lifestyle Tips for a Healthy Gut
Keeping your gut healthy when you have Type 2 Diabetes is more than just about diet. Lifestyle choices make a big difference. Practicing these simple tips each day can keep your digestive system in good shape and make diabetes management easier.
One of the key tips is to stay active. Regular exercise doesn't only help in managing diabetes, but it can also improve your gut health. Physical activity stimulates the muscles in your digestive tract, which helps in moving food through your system. As a result, you can avoid constipation and other digestive issues. Even a brisk 30-minute walk a day can work wonders.
Hydration is another crucial factor. Drinking enough water is essential for digestion. Water helps dissolve nutrients and minerals, making them more accessible to the body. It also softens food, helping it move more easily through the intestines. Aim to drink at least 8 cups of water daily, and remember that fluids can come from sources other than water, like fresh fruits and soups.
Managing stress is often overlooked, but it greatly impacts gut health. The gut and brain are connected through the gut-brain axis. Stress can disrupt this connection, leading to digestive problems like bloating, diarrhea, or an upset stomach. Practicing relaxation techniques, such as deep breathing, meditation, or yoga, can help in reducing stress levels. One study found that mindful meditation may reduce digestive symptoms and improve the quality of life for people with digestive issues.
“Taking time to relax and manage stress is not just good for your mind, but also for your gut,” says Dr. Michael Gershon, a neurogastroenterologist.
Sleep also plays a significant role in gut health. Poor sleep patterns can disrupt the balance of gut bacteria, leading to digestive issues. Strive for 7-9 hours of quality sleep every night. Create a bedtime routine, keep your bedroom dark and cool, and avoid screens an hour before bed to improve sleep quality.
Incorporating probiotics and prebiotics into your diet can also support a healthy gut. Probiotics are beneficial bacteria that help maintain gut health and are found in fermented foods like yogurt, sauerkraut, and kimchi. Prebiotics are fibers that probiotics feed on, found in foods like garlic, onions, and bananas. Ensuring you have enough of both in your diet can help keep your gut flora balanced and healthy.
Finally, eating slowly and mindfully can improve digestion. Taking the time to chew your food thoroughly can aid digestion and give your guts enough time to process what's coming in. Eating in a calm, relaxed environment can also help prevent indigestion caused by eating too quickly.



20 Comments
Andrew Butler-17 May 2024
Let’s be real-gut health isn’t some mystical new-age fad. It’s microbiome science, and if you’re not optimizing for SCFAs like butyrate, you’re just winging it with your glucose control. The dysbiosis-diabetes link is peer-reviewed, not anecdotal. Stop eating processed crap and start feeding your flora. Fiber isn’t optional-it’s metabolic medicine. And yes, I’m talking to you, the guy who thinks sugar-free soda is a healthy choice. It’s not. Artificial sweeteners mess with your gut microbiota and insulin signaling. Read the papers, not the marketing.
Varun Gupta-19 May 2024
lol they just want you to buy probiotic supplements 😂 the real cure is eating like your grandma did. no labels. no science. just food. 🍚🥬
Amy Reynal-19 May 2024
Okay but can we talk about how everyone’s acting like this is brand new info? My abuela in Puerto Rico was eating fermented naranja peel and black beans with rice before most of us were born. Fiber? She called it ‘el limpiador natural.’ Probiotics? She called it ‘la buena bacteria.’ And she lived to 92 with a HbA1c of 5.8. We’ve forgotten how to eat like humans. We’re not lab rats. We’re not algorithms. We’re cultural beings who evolved with whole foods, not isolated nutrients. So yes, science backs it-but so did tradition. And tradition didn’t need a grant to know that sugar kills your gut. Also, hydration isn’t just water. It’s broth. It’s herbal tea. It’s eating your vegetables, not just swallowing a capsule. And if you’re stressed? Your gut knows. Your gut remembers. Your gut holds trauma. So breathe. Chew slowly. Eat with joy. It’s not just about glucose-it’s about belonging.
Lidia Hertel-19 May 2024
YES. This. I’ve been doing the high-fiber, low-sugar, fermented-food thing for 3 years now and my A1c dropped from 7.8 to 5.9. No meds changed. Just food. And sleep. And walking after dinner. I used to think ‘gut health’ was just for people with IBS, but no-it’s the hidden engine of insulin sensitivity. I started with kimchi (spicy, so I cried the first bite) and now I make my own sauerkraut. It’s weird, but it’s mine. And my stomach doesn’t feel like a warzone anymore. Also, stop drinking diet soda. It’s not helping. I promise. 🙏
Chris Bock-20 May 2024
The gut is the second brain. And it’s mad.
Alyson Knisel-21 May 2024
i used to think fiber was just for ‘regularity’ but then my blood sugar stopped spiking after oatmeal and i realized-oh. it’s not about pooping. it’s about control. like, actual control. over my body. over my cravings. over the chaos. i don’t know if it’s science or magic but i’ll take it. also, i still eat cookies. just not every day. and i chew them like they’re a gift.
Jelisa Cameron- Humphrey-22 May 2024
Let’s not reduce this to ‘eat more fiber.’ The gut microbiome is a complex ecosystem. You’re not just feeding bacteria-you’re modulating immune pathways, epigenetic expression, and even neurotransmitter production. Butyrate from fiber fermentation upregulates GLP-1, which enhances insulin secretion and satiety. Probiotics like L. reuteri and B. adolescentis have shown in RCTs to reduce fasting glucose. Prebiotic oligosaccharides modulate bile acid metabolism. This isn’t wellness fluff. It’s systems biology. And if you’re not tracking your microbial diversity via stool tests or at least monitoring inflammatory markers, you’re flying blind. Don’t just ‘try’-optimize.
Lee Lach-24 May 2024
Let’s cut through the noise. This entire post is a corporate-sponsored distraction. Big Pharma doesn’t want you healing your gut-they want you buying metformin, insulin, and probiotic supplements. The real cause of Type 2 Diabetes? Chronic hyperinsulinemia from processed carbohydrates and seed oils. The gut is a symptom, not the source. Fix the insulin, fix the gut. Stop chasing bacteria like they’re magic beans. Eat meat. Eat fat. Eat vegetables. Don’t eat grain. Don’t eat sugar. Don’t eat ‘fiber supplements.’ Your ancestors didn’t need kimchi to survive. They ate what was available. And they didn’t have diabetes. The microbiome is irrelevant if your insulin is out of control. This is a distraction. A placebo dressed in science.
Tracy McKee-24 May 2024
everyone says fiber but no one says how much and when and what kind and if you’re doing it wrong you’re just feeding bad bacteria and making it worse so stop pretending you know what you’re doing
Abigail M. Bautista-26 May 2024
i tried the kimchi. didn’t like it. back to my rice cakes.
Rohan Puri-27 May 2024
fiber? really? in india we eat roti and rice every day and still get diabetes so what’s the point
Mandeep Singh-27 May 2024
this is western nonsense. our grandmothers didn’t eat yogurt. they ate jaggery and ghee. and they were healthy. why are you copying americans?
Chris Bellante-28 May 2024
Man, I’m Nigerian and we’ve always known-when your belly is quiet, your blood is calm. We don’t call it ‘gut health.’ We call it ‘the inside working right.’ Eaten pounded yam with bitterleaf soup for 40 years. No probiotics. No labels. Just food that remembers you. Fermented ogi? That’s prebiotic. Palm oil? Anti-inflammatory. Coconut water? Hydration with electrolytes. We didn’t need a journal to tell us this. We just lived. But now? People overcomplicate it. Eat real. Move real. Breathe real. The rest? Marketing.
Nicole Manlapaz-29 May 2024
you guys are making this so heavy. it’s not rocket science. eat veggies. walk after meals. drink water. sleep. don’t stress about the perfect probiotic strain. just start somewhere. i started with one banana a day. now i eat 3. my sugar’s better. my mood’s better. my pants fit better. that’s it. no science degree needed. just consistency. and maybe a little patience. you got this. 🌱💖
Frederick Staal-31 May 2024
And yet, despite all this ‘gut health’ rhetoric, the CDC reports that Type 2 Diabetes incidence continues to rise. Coincidence? Or is this entire narrative a well-funded distraction from the real issue: systemic dietary policy failure and industrial food manipulation? You can’t probiotic your way out of a food environment designed to addict you. The gut is not broken. The system is. And until we address the food industry’s role in chronic disease, we’re just rearranging deck chairs on the Titanic. Your kimchi won’t save you if your city has no grocery store. Your fiber won’t help if your paycheck won’t cover it. This is privilege dressed as wellness.
erin orina- 1 June 2024
i just wanted to say thank you for writing this. i’ve been scared to talk about my diabetes because i feel like i’m failing. but reading this made me feel like maybe i’m not alone. i started eating lentils last week. i’m not perfect. i still crave sweets. but i’m trying. and that’s enough. 🫂
Lisa Uhlyarik- 3 June 2024
why are you all so obsessed with your guts? it’s just poop. you’re all acting like your microbiome is your soul. get a life.
Kelley Akers- 4 June 2024
How quaint. You all think fiber and kimchi are the answers. But have you considered that the real issue is the collapse of ancestral dietary patterns? The Western diet is a metabolic poison. You’re not healing your gut-you’re performing performative wellness. Real health isn’t Instagrammable. It’s quiet. It’s consistent. It’s not buying a $40 probiotic jar. It’s growing your own kale. It’s fermenting your own vegetables. It’s rejecting convenience. It’s rejecting the myth that health can be commodified. You’re not fixing your gut. You’re buying into capitalism’s latest scam.
JOANNA WHITE- 5 June 2024
just ate a big bowl of oatmeal with chia and blueberries. felt like my insides were singing. also walked 20 mins after. no meds. just food. and time. 🌿
Peggy Cai- 6 June 2024
fiber is overrated and you’re all just scared to admit sugar is the real problem