When you’re taking a pill to control your blood sugar, the last thing you want is for it to drop too low. But for many people on sulfonylureas, that’s exactly what happens. These older diabetes drugs are cheap, effective, and still prescribed to millions - but they come with a serious catch: hypoglycemia. Low blood sugar isn’t just a nuisance. It can mean shaking, sweating, confusion, or worse. And for some, it lands them in the hospital.
Why Sulfonylureas Cause Low Blood Sugar
Sulfonylureas work by forcing your pancreas to release insulin - no matter what your blood sugar level is. That’s the problem. Your body doesn’t get to decide when it needs insulin. The drug does. So even if you skip a meal, go for a walk, or sleep through the night, your pancreas keeps pumping out insulin. That’s why blood sugar can crash without warning. The most common sulfonylureas are glyburide, glipizide, glimepiride, and gliclazide. But not all are created equal. Glyburide, the most prescribed in the U.S., has a long half-life - up to 10 hours - and its metabolites stick around even longer. That means it’s active in your body for most of the day and night. Glipizide? Shorter-acting. Clears faster. Less chance of a midnight low. Studies show glyburide causes nearly 40% more severe hypoglycemia than glipizide. In one study, people on glyburide had 1.8 hospitalizations per 100 person-years. Those on glipizide? Only 1.2. That’s a big difference when you’re trying to stay out of the ER.Who’s Most at Risk?
Age matters. People over 65 are at higher risk - not just because their bodies process drugs slower, but because their counter-regulatory responses weaken. But here’s something surprising: not all older adults are equally vulnerable. One 1998 study found that healthy elderly patients on sulfonylureas still released epinephrine (the stress hormone that helps raise blood sugar) when levels dropped - meaning their bodies were still fighting back. The real danger? Those with kidney problems, irregular eating habits, or who take other medications that interact with sulfonylureas. Drugs like gemfibrozil (for cholesterol), sulfonamide antibiotics, and even warfarin can push sulfonylureas out of their protein-binding sites in the blood. That means more free drug floating around - and a bigger insulin spike. One study showed gemfibrozil increases glyburide levels by 35%. That’s not a small bump. That’s a red flag. Genetics play a role too. If you carry the CYP2C9*2 or *3 gene variant, your body breaks down sulfonylureas slower. That means higher drug levels, longer action, and a 2.3 times greater risk of low blood sugar. It’s not something your doctor checks by default - but it should be.Real People, Real Low Blood Sugar Stories
Online forums are full of stories. On Reddit, one user wrote: “Switched from metformin to glyburide last month. Had three severe lows requiring glucagon. My doctor didn’t warn me this could happen multiple times a week.” Another user on DiabetesDaily.com shared: “I switched from glyburide to glipizide. My lows went from weekly to once every two months.” These aren’t outliers. A review of over 1,200 posts on the American Diabetes Association’s community showed 68% of sulfonylurea users had at least one hypoglycemic episode. Over 20% needed help from someone else - because they were too confused or unconscious to treat it themselves.
How to Prevent Low Blood Sugar
The good news? You can cut your risk - a lot. Start low, go slow. Doctors should begin with the smallest possible dose: 1.25 mg of glyburide, or 2.5 mg of glipizide. Too many people start at 5 mg or higher. That’s asking for trouble. A 2022 survey found 78% of endocrinologists now follow this cautious approach. Switch to a safer sulfonylurea. If you’re on glyburide, ask about glipizide or glimepiride. Gliclazide - not available in the U.S. but widely used in Australia and Europe - has the lowest hypoglycemia risk among all sulfonylureas because it targets only pancreatic beta cells, not other tissues. Don’t skip meals. This sounds obvious, but it’s the #1 trigger. Even a light snack before bed can prevent overnight lows. If you’re active, eat before or after exercise. Sulfonylureas don’t care if you’re walking or sleeping - they’re still pushing insulin out. Use a continuous glucose monitor (CGM). A 2022 trial showed that sulfonylurea users wearing CGMs had 48% less time spent in low blood sugar. You get alerts before you feel shaky. You can see trends. You can adjust before it becomes an emergency. Know the signs. Sweating (85% of cases), shaking (78%), hunger (41%), irritability (65%) - these aren’t just symptoms. They’re your body’s alarm system. If you feel any of these, check your blood sugar. Don’t wait. Don’t hope it’ll pass. Treat it fast. If your blood sugar is below 70 mg/dL, take 15 grams of fast-acting carbs: 4 glucose tablets, ½ cup juice, or 1 tablespoon of honey. Wait 15 minutes. Check again. Repeat if needed. Then eat a snack with protein and carbs to keep it stable.What About Newer Drugs?
Newer diabetes medications - SGLT2 inhibitors, GLP-1 agonists, DPP-4 inhibitors - have much lower hypoglycemia rates. Some have fewer than 0.3 episodes per 100 person-years. That’s 5 to 6 times lower than sulfonylureas. But here’s the catch: they’re expensive. Glipizide costs about $4 a month. A GLP-1 agonist can cost $800. For many people, especially those without good insurance, cost matters. That’s why sulfonylureas are still prescribed - even as their use drops. A 2021 study found sulfonylureas save $1,200-$1,800 per patient annually compared to newer drugs - while bringing HbA1c down just as much. So it’s not about which drug is better. It’s about which drug is right for you.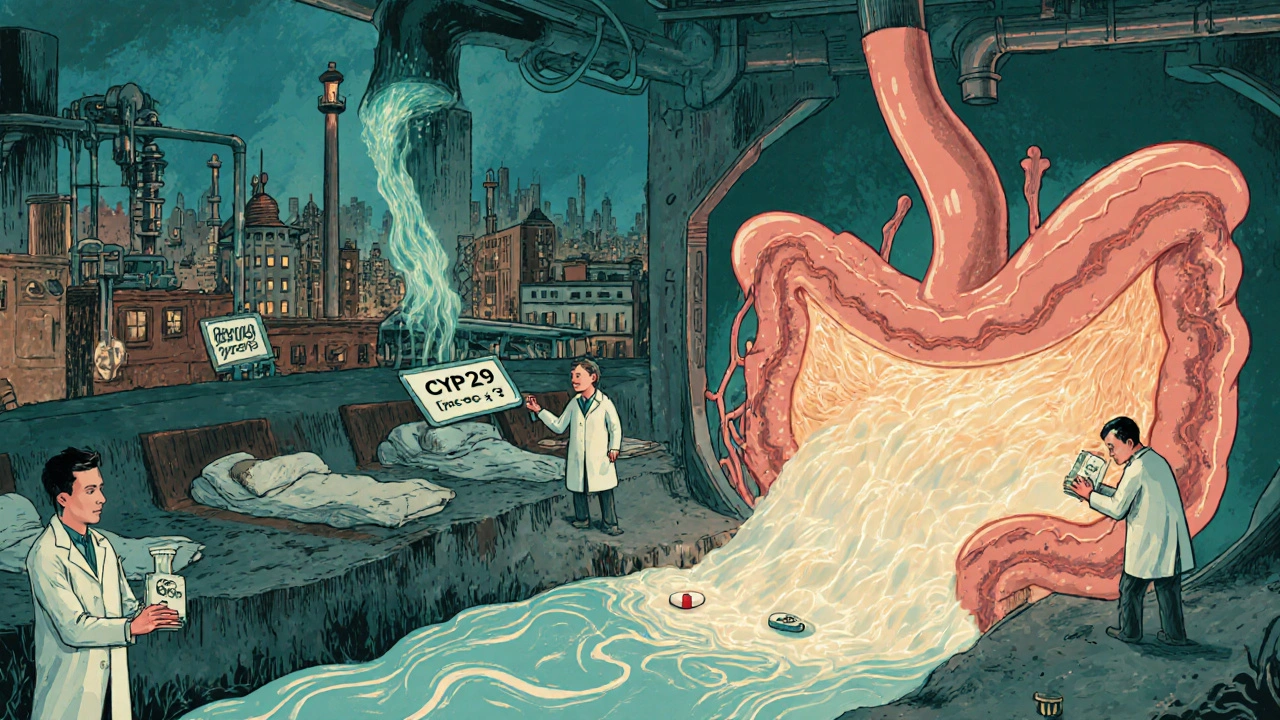





12 Comments
Alexander Levin-30 November 2025
This whole post is just Big Pharma whispering sweet nothings into your doctor's ear. 😏 Sulfonylureas? More like 'sulfo-ruin-your-life'. I switched to metformin after my third ER trip. They don't want you to know about the cheaper, safer stuff.
Sue Barnes- 1 December 2025
If you're still on glyburide after reading this, you're either a masochist or your doctor is on the pharmaceutical payroll. 🤦♀️ Start low, go slow? Why are we even having this conversation in 2025?
jobin joshua- 3 December 2025
Bro, I'm from India and we use gliclazide all the time here. No drama. No midnight lows. 😎 Try it if your doc is too lazy to switch you. And yes, I'm not sponsored. Just survived 12 years on this.
Sachin Agnihotri- 4 December 2025
I just wanted to say... thank you for writing this. 🙏 I was on glyburide for 3 years, had 7 hypoglycemic episodes, and my doc just said 'it's normal'. I switched to glipizide last month and my life changed. No more panic attacks before bed. You're not alone.
Diana Askew- 6 December 2025
CGMs are $1000 a month. You think I can afford that? 😒 Meanwhile, glipizide costs less than my morning coffee. Don't act like everyone lives in your fancy Silicon Valley bubble.
King Property- 7 December 2025
Let me break this down for the 78% of you who didn't read the whole thing: Glyburide = slow poison. Glipizide = better option. Gliclazide = gold standard. CYP2C9 testing = mandatory. If your doc doesn't know this, fire them. This isn't 1998 anymore.
Yash Hemrajani- 7 December 2025
Oh wow, a 2022 study says you should start low? Shocking. 😏 Meanwhile, my cousin in Delhi got prescribed 10mg of glyburide on day one. He passed out at the bus stop. Guess who got blamed? 'You didn't eat enough.' No, doc. You didn't know your job.
Pawittar Singh- 8 December 2025
Hey everyone, I know this stuff feels overwhelming 😔 But hear me out - you're not broken. Your meds are just outdated. Talk to your doctor. Ask about glimepiride. Try a CGM for a week. Even if you can't afford it, ask for samples. You deserve to feel safe. 💪 We got you.
Josh Evans-10 December 2025
I switched from glyburide to glipizide last year. Zero lows since. My HbA1c is 6.1. I'm not even trying. Just switched drugs. Why is this not standard practice?
Allison Reed-11 December 2025
The fact that we still need to argue about this in 2025 is terrifying. Sulfonylureas are not obsolete because they're ineffective - they're obsolete because they're dangerous. And yet, they're still first-line in 40% of U.S. clinics. We need better guidelines, not just better patients.
Jacob Keil-11 December 2025
CYP2C9 testing? That's like asking your doctor to read a book. 😅 They just wanna write a script. I'm 62, diabetic, and my doc still thinks 'just eat more sugar' is a solution. We're not patients. We're profit margins.
Rosy Wilkens-13 December 2025
I'm a nurse. I've seen 14 patients in the last year with diabetic ketoacidosis triggered by sulfonylurea-induced hypoglycemia. The ER staff rolls their eyes when they see the script: 'glyburide 5mg daily'. This isn't medicine. It's negligence dressed in white coats.