More than 500 million people worldwide live with type 2 diabetes. And for most of them, the story didn’t start with high blood sugar-it started with something quieter, less visible: insulin resistance. This isn’t just a buzzword. It’s the hidden engine driving the rise of metabolic syndrome, prediabetes, and eventually full-blown type 2 diabetes. If you’ve ever felt exhausted after eating, struggled to lose weight no matter how hard you tried, or been told your waist size is a red flag, you’re not alone. These aren’t just inconveniences-they’re early warning signs your body is losing its ability to handle sugar.
What Exactly Is Insulin Resistance?
Insulin is the hormone your pancreas makes to tell your cells: "Take in glucose from the blood." Think of it like a key unlocking a door so sugar can enter muscle, fat, and liver cells to be used for energy. In insulin resistance, those locks start to rust. The keys still turn, but not as well. Cells don’t respond the way they should. Sugar stays in the bloodstream instead of being used.
This isn’t a sudden event. It builds slowly. Years of eating too many refined carbs, sitting too much, and carrying extra belly fat cause fat cells to release inflammatory signals. These signals interfere with insulin’s signaling pathway-specifically the IRS-1/PI3K/Akt2 chain-making cells blind to insulin’s message. The pancreas notices the rising blood sugar and pumps out more insulin to compensate. This is called hyperinsulinemia. You might have high insulin for a decade before your blood sugar finally climbs into the danger zone.
By the time fasting glucose hits 100 mg/dL, you’re already in prediabetes. At 126 mg/dL or higher, you’re diagnosed with type 2 diabetes. But the real damage? It started years before that number showed up on a lab report.
Metabolic Syndrome: The Cluster That Signals Trouble
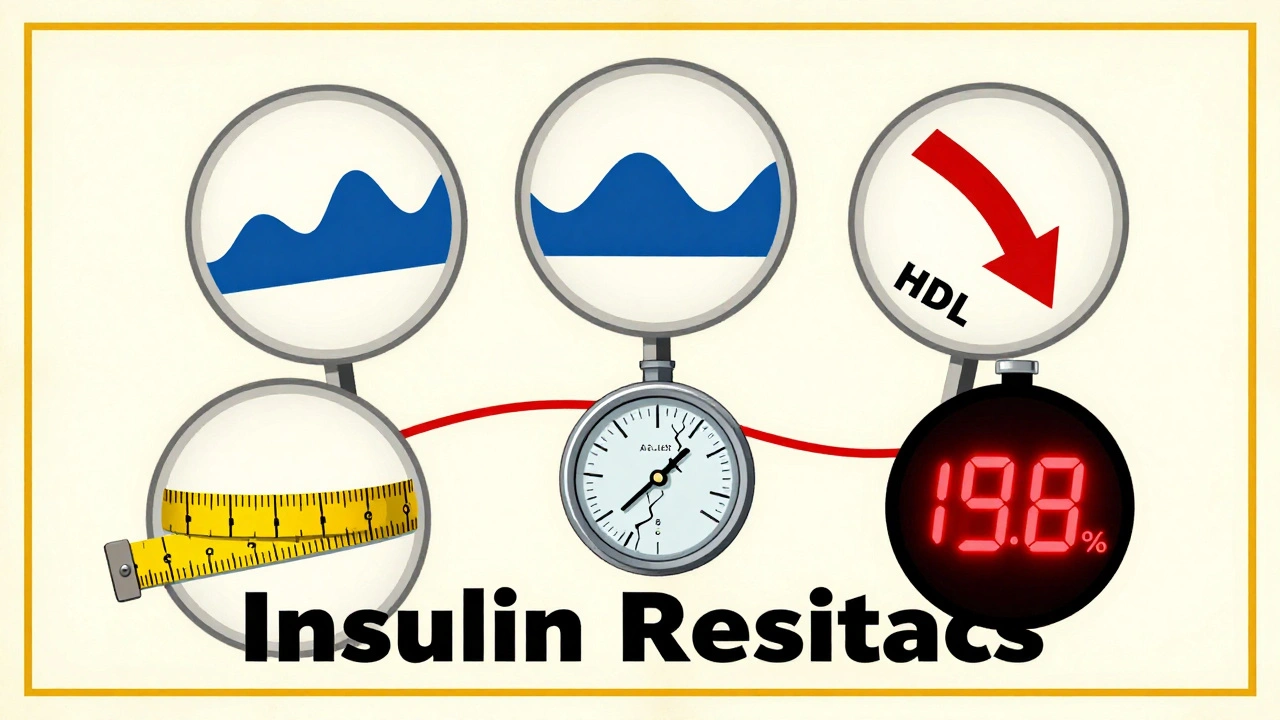
Metabolic syndrome isn’t one disease. It’s a group of five warning signs that often show up together:
- Waist circumference over 94 cm (37 inches) for men, 80 cm (31.5 inches) for women
- Triglycerides above 150 mg/dL
- HDL cholesterol below 40 mg/dL (men) or 50 mg/dL (women)
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
You only need three of these to be diagnosed. And if you have them, your risk of heart disease jumps 200-300%. Your chance of developing type 2 diabetes? Five to six times higher than someone without any of these signs.
Here’s the catch: not everyone who’s overweight has metabolic syndrome. And not everyone with metabolic syndrome is overweight. It’s about where the fat is stored. Belly fat-especially fat inside the abdomen and liver-is far more dangerous than fat on the hips or thighs. That fat isn’t just storage. It’s active, releasing chemicals that worsen insulin resistance and inflammation.
Doctors are starting to call this condition metabolic dysfunction syndrome instead of metabolic syndrome. Why? Because it’s not just a cluster of numbers-it’s a broken system. The body’s metabolism is failing, not just showing odd readings.
The Link Between Insulin Resistance and Metabolic Syndrome
Insulin resistance doesn’t just affect blood sugar. It messes with fat, blood pressure, and cholesterol too.
When your liver becomes resistant to insulin, it stops turning off glucose production. Even when you haven’t eaten, it keeps dumping sugar into your blood. At the same time, your fat cells break down stored fat faster, flooding your bloodstream with fatty acids. These fats get dumped into your liver and muscles, creating what’s called ectopic fat-fat where it shouldn’t be. That’s how nonalcoholic fatty liver disease (NAFLD) develops. And NAFLD? It doubles your risk of type 2 diabetes.
High insulin levels also cause your kidneys to hold onto sodium, which raises blood pressure. And because insulin suppresses a key enzyme that clears triglycerides, your levels climb while HDL-the "good" cholesterol-plummets.
This isn’t coincidence. It’s cause and effect. Insulin resistance is the common thread tying together high blood pressure, belly fat, bad cholesterol, and rising sugar. That’s why experts like Dr. Ralph DeFronzo call it the "single most important pathophysiological defect" leading to type 2 diabetes.
Who’s at Risk? It’s Not Just About Weight
Yes, obesity increases risk. But genetics play a huge role. People of South Asian, African, or Indigenous descent often develop insulin resistance at lower body weights. Lean individuals with visceral fat and fatty liver can have metabolic syndrome-even if their BMI is normal.
Age matters. After 45, your muscle mass naturally declines, making your body less able to use glucose. Inactivity makes it worse. A sedentary job, long hours sitting, and skipping movement all add up.
And sleep? Poor sleep or sleep apnea raises cortisol and inflammation, both of which worsen insulin resistance. Stress does too. Chronic stress keeps your body in "fight or flight," flooding it with glucose and adrenaline, making insulin work harder.
One study found that 78% of people with metabolic syndrome report constant fatigue and trouble losing weight. Another 65% say they feel hungry even after eating. That’s because high insulin blocks the brain’s signal that you’re full. You’re not weak-you’re fighting a hormonal storm.
Can You Reverse It?
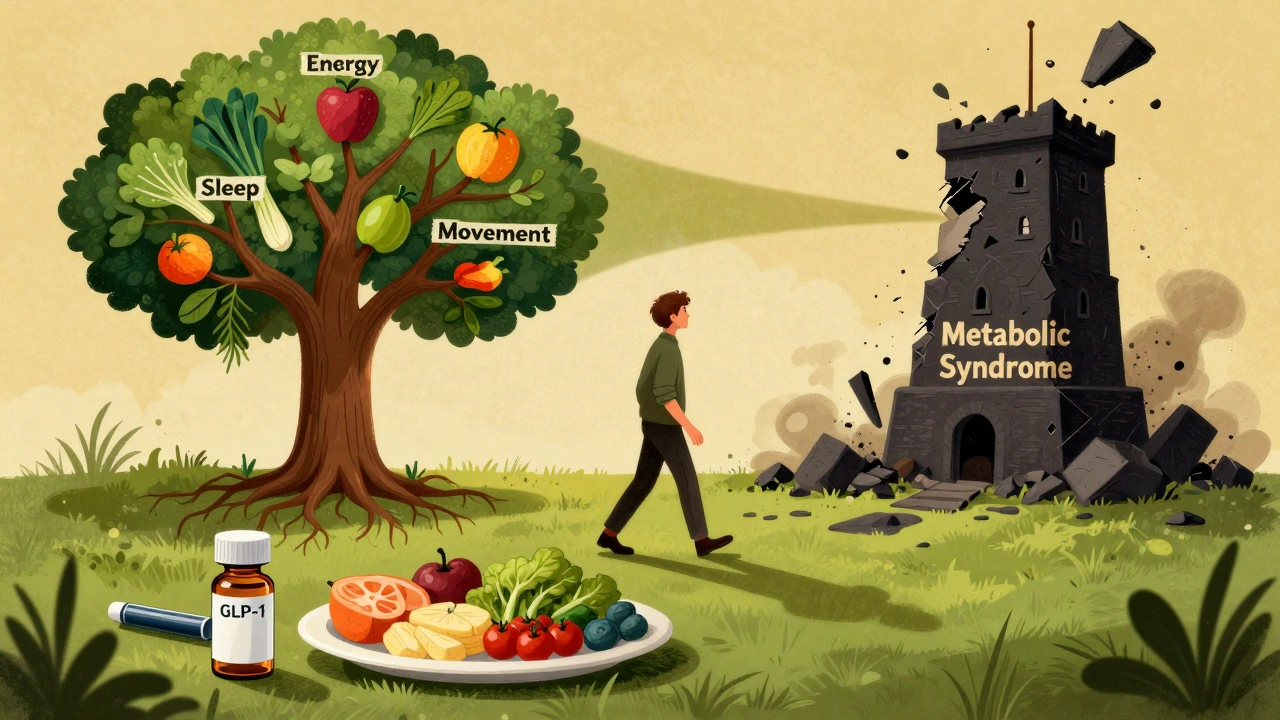
Yes. And not just slow it down-reverse it.
The Diabetes Prevention Program (DPP) showed that losing just 7% of your body weight and getting 150 minutes of walking per week cut diabetes risk by 58%. That’s more effective than metformin, the most common diabetes medication.
What works?
- Move more. Strength training twice a week builds muscle, which soaks up glucose. Walking after meals helps lower blood sugar spikes.
- Eat real food. Cut out sugary drinks, white bread, pastries, and processed snacks. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats like olive oil and avocado.
- Sleep 7-8 hours. Fixing sleep apnea can dramatically improve insulin sensitivity.
- Manage stress. Meditation, deep breathing, or even time in nature can lower cortisol and inflammation.
Some people need medication. Metformin is still the first-line choice for prediabetes with metabolic syndrome. It reduces liver glucose output and improves insulin sensitivity. Newer drugs like semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro) don’t just lower blood sugar-they cause significant weight loss, reduce liver fat, and even reverse early diabetes in many cases.
In the STEP trials, people lost nearly 15% of their body weight on semaglutide. In the SELECT trial, 66% of those with type 2 diabetes achieved remission after using tirzepatide. These aren’t magic pills-they’re tools. But they work best when paired with lifestyle changes.
What Happens If You Ignore It?
Left unchecked, insulin resistance doesn’t just become type 2 diabetes. It becomes heart attack, stroke, kidney failure, nerve damage, vision loss, and amputation. The CDC predicts that by 2050, one in three Americans will have diabetes. That’s not inevitable. It’s a policy failure, a public health crisis, and a personal wake-up call.
But here’s the hopeful part: the same lifestyle changes that reverse insulin resistance also reduce inflammation, lower blood pressure, improve cholesterol, and protect your brain and heart. You’re not just preventing diabetes-you’re reclaiming your energy, your mood, and your future.
What Should You Do Next?
Start with these three steps:
- Get your waist measured. If it’s over 94 cm (men) or 80 cm (women), talk to your doctor.
- Ask for a fasting glucose and HbA1c test. If your HbA1c is 5.7% or higher, you’re in prediabetes.
- Start walking 20 minutes after dinner every day. That’s it. No gym required. No expensive supplements.
You don’t need to overhaul your life overnight. Just begin. One small change, repeated daily, can break the cycle of insulin resistance before it breaks your health.
Is metabolic syndrome the same as type 2 diabetes?
No. Metabolic syndrome is a group of risk factors-like high blood sugar, belly fat, high triglycerides, and high blood pressure-that often lead to type 2 diabetes. You can have metabolic syndrome without diabetes, but if you do, your chance of developing diabetes is five to six times higher.
Can you have insulin resistance without being overweight?
Yes. While obesity increases risk, people of normal weight-especially those of South Asian, African, or Indigenous descent-can have high levels of visceral fat and insulin resistance. Genetics, inactivity, and poor sleep can trigger it even without extra pounds.
Does metformin cure insulin resistance?
Metformin doesn’t cure it, but it helps. It reduces the liver’s glucose output and makes cells more sensitive to insulin. In the Diabetes Prevention Program, it lowered diabetes risk by 31%. But lifestyle changes were more effective-cutting risk by 58%. Medication supports, but doesn’t replace, healthy habits.
How long does it take to reverse insulin resistance?
Improvements can show up in weeks. Blood sugar and insulin levels often drop within 2-4 weeks of cutting sugar and starting daily movement. Meaningful weight loss and improved insulin sensitivity typically take 3-6 months. The Look AHEAD trial showed that people who lost 10% of their body weight in a year saw partial diabetes remission-and some maintained it for over 8 years.
Are GLP-1 drugs like Ozempic the future of treating metabolic syndrome?
They’re a powerful tool. Drugs like semaglutide and tirzepatide cause significant weight loss, reduce liver fat, and improve insulin sensitivity. In trials, over 60% of people with type 2 diabetes achieved remission. But they’re expensive, not always covered by insurance, and work best with diet and movement. They’re not a substitute for lifestyle-they’re an accelerator.
Final Thought: It’s Not About Perfection
You don’t need to eat perfectly. You don’t need to run marathons. You just need to move more than you did yesterday. Eat one less sugary snack. Take the stairs. Sleep an extra hour. These aren’t just "good habits." They’re medicine. And the best part? Your body responds fast. Within weeks, you’ll feel less tired. Your hunger will settle. Your clothes will fit better. And you’ll realize-you’re not just preventing diabetes. You’re getting your life back.




9 Comments
May .- 3 December 2025
This is why I stopped counting calories and just started walking after dinner. My waist shrunk before my scale did.
Sara Larson- 4 December 2025
YES. I was prediabetic and thought I was doomed. Started walking after meals + cutting out soda. 6 months later, my HbA1c dropped from 6.1% to 5.2%. 🙌 You don’t need a miracle-just consistency. I’m proof. 💪
Cristy Magdalena- 6 December 2025
I’ve been told I’m ‘just lazy’ for years. But no one ever told me my insulin was screaming. This article? It finally made me feel seen. I cried reading it. Not because I’m weak-because I finally understood what was happening inside me. 🫂
Josh Bilskemper- 7 December 2025
The DPP data is solid but overhyped. Most people can’t maintain 150 minutes of walking weekly. The real solution is pharmaceutical intervention. Lifestyle changes are for people who have time and privilege. The rest of us need GLP-1s. End of story.
Tom Costello- 9 December 2025
I’m a Filipino-American and grew up eating rice with every meal. I was lean but had fatty liver and high triglycerides at 38. No one ever connected it to insulin resistance. This article nailed it. Genetics + culture + sedentary job = perfect storm. Glad someone’s talking about this without shaming.
kelly mckeown-10 December 2025
i just started reading this and i feel like someone finally gets it. i dont even know why i kept eating sugar even though i felt awful after. now i think it was my body screaming for help. i started walking with my dog after dinner and honestly? i sleep better. thank you for writing this.
dylan dowsett-12 December 2025
You people are delusional. Walking after dinner? That’s not medicine-that’s a placebo for people who don’t want to face reality. If you’re insulin resistant, you need metformin. Period. And if you’re too lazy to take it, don’t pretend your ‘lifestyle changes’ are saving you. You’re just delaying the inevitable.
Susan Haboustak-13 December 2025
You’re all ignoring the real issue: systemic food deserts and corporate manipulation of the food supply. No amount of walking will fix insulin resistance if you live in a neighborhood where the only ‘healthy’ option is a $7 pre-packaged salad that’s 70% sugar. This article is a luxury for the privileged. The rest of us are just surviving.
Sara Larson-13 December 2025
To the person who said walking isn’t medicine: I used to think that too. Then I lost 18 lbs, my blood pressure dropped 20 points, and my doctor said I’m no longer prediabetic. I didn’t need a pill-I needed to move. And I’m not privileged-I work two jobs and still walk after dinner. It’s not about perfection. It’s about showing up. 🌱