Uveitis isn’t just a red eye. It’s inflammation deep inside your eye - in the uvea, the middle layer that feeds your retina and iris. Left untreated, it can blur your vision, cause permanent damage, and even lead to blindness. This isn’t rare. It’s the third leading cause of vision loss worldwide. If you’ve had sudden eye redness, pain when reading, or floaters that won’t go away, you need to know what’s happening - and what to do next.
What Exactly Is the Uvea?
The uvea isn’t one part. It’s three layers stacked together: the iris (the colored part), the ciliary body (which controls lens focus and fluid production), and the choroid (a blood-rich layer behind the retina). Together, they supply oxygen and nutrients to the eye’s most sensitive tissues. When inflammation hits any of these, it’s uveitis. The location determines the symptoms, severity, and treatment.Four Types of Uveitis - And How They Feel
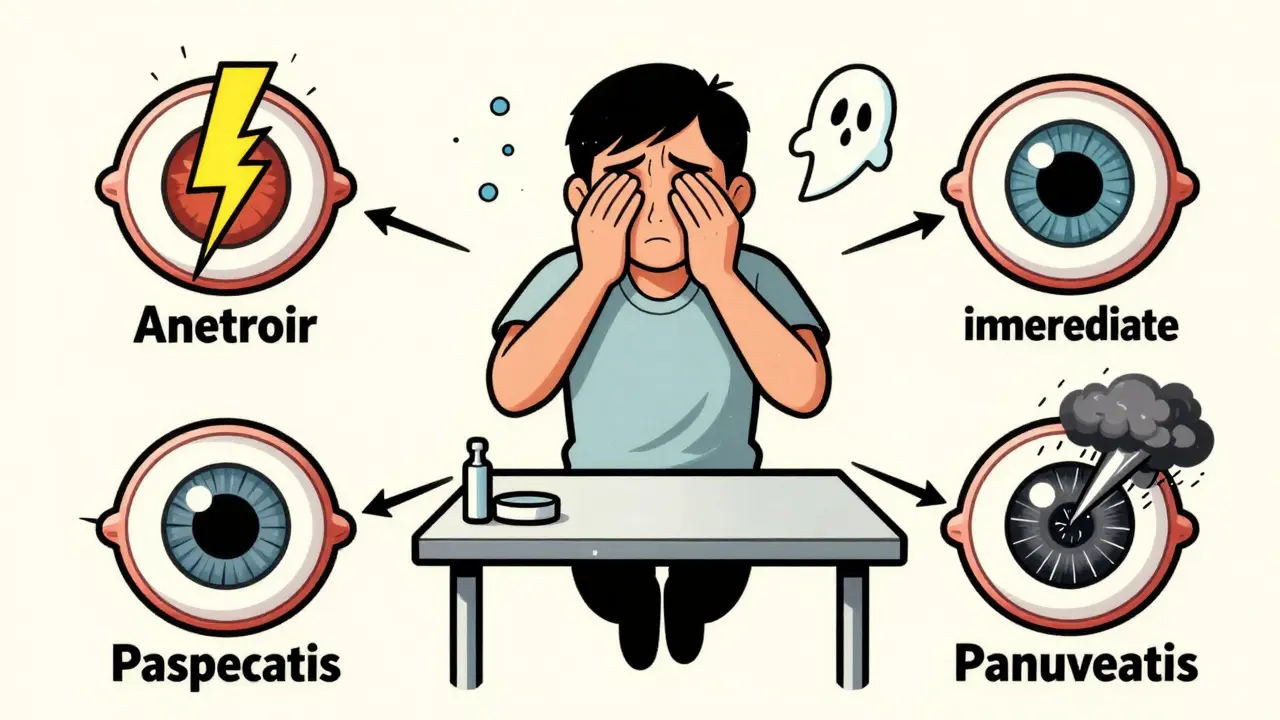
Uveitis isn’t one condition. It’s four, each with different signs and risks.- Anterior uveitis (iritis) is the most common - about 75-90% of cases. It hits the front: iris and ciliary body. You’ll know it. Your eye turns blood-red. Light hurts. You can’t read without squinting. Pain is sharp, often worse when focusing. This type comes on fast - sometimes in hours. It usually affects one eye, but can spread.
- Intermediate uveitis (pars planitis) targets the vitreous, the jelly-like fluid behind the lens. Symptoms are subtler: floaters, blurred vision, no pain. It’s sneaky. People think it’s just tired eyes. But it often becomes chronic, lasting years with flare-ups. Macular edema - swelling in the center of your vision - is a big risk here.
- Posterior uveitis attacks the retina and choroid. This is the most dangerous. Vision loss happens slowly, often in both eyes. You might not notice until it’s advanced. It’s frequently diagnosed during a routine eye exam because symptoms don’t scream for attention. Retinal scarring and optic nerve damage are real threats.
- Panuveitis hits all layers at once. It’s the worst-case scenario. You get redness, pain, floaters, blurred vision - everything. It’s linked to serious autoimmune or infectious diseases. Recovery is harder, and complications are common.
What Causes Uveitis? Most Cases Have No Clear Answer
You’d think doctors could point to a virus, an injury, or a disease. But here’s the hard truth: in about half to two-thirds of cases, the cause is unknown. That’s idiopathic uveitis. No test finds it. No blood work explains it. When there is a cause, it falls into three buckets:- Autoimmune diseases: Ankylosing spondylitis, sarcoidosis, multiple sclerosis, lupus. Your immune system attacks your own eye tissue, thinking it’s foreign.
- Infections: Herpes simplex, shingles (herpes zoster), cytomegalovirus, syphilis, toxoplasmosis. These germs trigger inflammation as they try to hide in the eye.
- Trauma or surgery: A blow to the eye, a scratch, or even an eye operation can spark inflammation as the body tries to heal.
Steroid Therapy: The First Line of Defense
There’s no magic cure. But there’s one treatment that works across all types: steroids. Corticosteroids are powerful anti-inflammatories. They shut down the immune system’s overreaction in the eye. How you get them depends on where the inflammation lives:- Anterior uveitis: Eye drops. Prednisolone acetate 1% is standard. You might start with drops every hour, then taper over weeks. The goal? Kill inflammation fast, then stop before side effects start.
- Intermediate uveitis: Drops don’t reach deep enough. You need injections around the eye (periocular) or oral steroids like prednisone. Some patients get implants that slowly release steroids inside the eye for months.
- Posterior uveitis: Oral steroids are common. For severe cases, intravitreal implants (like Ozurdex) deliver steroids directly into the vitreous. This avoids whole-body exposure.
- Panuveitis: Usually requires systemic steroids - pills or IV - because the inflammation is everywhere.
The Hidden Cost of Steroids
Steroids save vision - but they can hurt it too. Long-term use, especially oral steroids, carries risks:- Cataracts: Clouding of the lens. Happens in up to 40% of patients on long-term steroids.
- Steroid-induced glaucoma: Pressure builds inside the eye. If unchecked, it damages the optic nerve - permanently.
- Systemic side effects: Weight gain, mood swings, high blood sugar, bone thinning. These are real for people on pills for months.
When to See a Doctor - Right Now
You don’t need to wait for a routine checkup. If you have any of these, go to an eye specialist today:- Sudden redness in one or both eyes
- Pain that gets worse when reading or focusing
- Floaters that won’t fade - especially if they multiply
- Blurred vision that doesn’t clear with glasses
- Extreme sensitivity to light - even indoors
What Happens If You Ignore It?
Untreated uveitis doesn’t just fade. It destroys. - Adhesions: The iris sticks to the lens or retina. This distorts the pupil and blocks fluid flow, raising eye pressure. - Macular edema: Swelling in the central retina. This blurs your ability to read, drive, or recognize faces. - Glaucoma: Permanent nerve damage from high pressure. - Cataracts: Clouded lenses from steroid use or inflammation. - Retinal detachment: In posterior uveitis, inflammation can pull the retina loose. - Permanent vision loss: Especially in posterior uveitis and panuveitis. Once the retina or optic nerve is scarred, vision won’t come back. The Lions Eye Institute calls uveitis a “potentially sight-threatening problem.” That’s not fear-mongering. That’s medicine.
What to Expect at the Eye Doctor
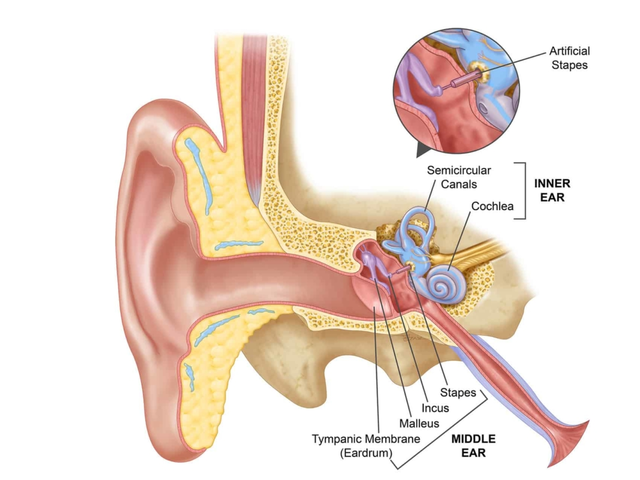
Your ophthalmologist won’t just look in your eye. They’ll investigate. - Slit-lamp exam: A microscope with bright light checks for cells and flare in the front of the eye. - Retinal exam: Pupil dilation lets them see the back of the eye - retina, choroid, optic nerve. - Eye pressure test: Glaucoma is a common complication. - Blood tests: For syphilis, sarcoidosis, Lyme, TB - if they suspect an infection or autoimmune cause. - Imaging: OCT scans show swelling in the macula. Fluorescein angiography checks blood flow in the retina. There’s no single test for uveitis. Diagnosis is a puzzle - symptoms, exam findings, and sometimes ruling out everything else.Can Uveitis Come Back?
Yes. Especially intermediate and posterior types. Some people have flare-ups every few months for years. That’s why long-term follow-up matters. Even if your eye looks fine, inflammation can be hiding. Regular checkups every 3-6 months are common for chronic cases. Your doctor will monitor pressure, vision, and retinal health. If you notice symptoms returning - even mildly - don’t wait. Call your eye doctor.Living With Uveitis
It’s not just about medicine. It’s about adaptation. - Wear UV-blocking sunglasses. Light sensitivity doesn’t go away overnight. - Avoid rubbing your eyes. Even gentle pressure can worsen inflammation. - Keep your overall health in check. Autoimmune conditions like ankylosing spondylitis need management too. - Talk to your doctor about steroid alternatives if you’re on pills long-term. - Join a support group. Chronic uveitis is isolating. You’re not alone. Vision recovery is possible - if treatment starts early. Many people with anterior uveitis regain full sight. But for those with posterior or chronic forms, the goal shifts: preserve what’s left. Prevent more loss.Bottom Line
Uveitis is not a minor eye irritation. It’s a serious, sight-threatening inflammation that demands immediate attention. Steroids are your best tool - but only if used right, at the right time, and with the right follow-up. If you have redness, pain, floaters, or sudden blurred vision, don’t wait. Don’t guess. See an eye specialist now. Your vision isn’t something you can afford to risk.Can uveitis go away on its own?
No. While mild cases might seem to improve temporarily, untreated uveitis almost always leads to complications like glaucoma, cataracts, or retinal damage. Even if symptoms fade, inflammation can continue silently. That’s why medical treatment is essential - not optional.
Are steroid eye drops safe for long-term use?
Short-term use under a doctor’s supervision is safe. But long-term use - more than a few weeks - raises the risk of cataracts and steroid-induced glaucoma. That’s why doctors taper the dose slowly and monitor eye pressure regularly. Never stop or restart drops on your own.
Can uveitis cause blindness?
Yes. Especially posterior uveitis and panuveitis. When inflammation damages the retina or optic nerve, vision loss can be permanent. That’s why early treatment is critical. The sooner you start steroids, the better your chances of saving your sight.
Is uveitis contagious?
No. Uveitis itself isn’t contagious. But if it’s caused by an infection like herpes or syphilis, those germs can spread. The eye inflammation is your body’s reaction - not something you can pass to someone else.
Can I wear contact lenses if I have uveitis?
No. During active inflammation, contact lenses increase the risk of infection and irritation. Your doctor will tell you when it’s safe to resume wearing them - usually only after inflammation has fully cleared and your eye is stable.
What’s the difference between uveitis and conjunctivitis?
Conjunctivitis (pink eye) affects the surface - the clear membrane over the white of the eye. It causes redness, discharge, and itchiness, but no pain or light sensitivity. Uveitis is deeper, inside the eye. It causes pain, blurred vision, and light sensitivity. Conjunctivitis is common and usually harmless. Uveitis is rare and dangerous.
Does stress cause uveitis?
Stress doesn’t cause uveitis, but it can trigger flare-ups in people who already have it - especially if they have an autoimmune condition. Managing stress won’t cure uveitis, but it can help reduce how often it comes back.


8 Comments
Alvin Bregman-15 January 2026
Been through this twice. First time thought it was allergies. Second time I knew better. Red eye + light sensitivity = go now. No waiting. My doc said if I’d waited another week I’d have been on steroids for a year instead of three months. Don’t be me.
Sarah Triphahn-16 January 2026
Typical medical system. Steroids fix the symptom but wreck your body. They don’t tell you this but every time you take prednisone, you’re basically telling your immune system ‘go away’ and it forgets how to work on its own. Welcome to lifelong dependency. You think uveitis is bad? Try living with steroid-induced diabetes and osteoporosis at 35.
Henry Sy-18 January 2026
Bro I had posterior uveitis and let me tell you it’s like your eyeball got possessed. No pain? Yeah right. It’s just the kind of pain that whispers in your skull while you’re trying to read a text. I got the Ozurdex implant. Felt like a sci-fi movie. One shot and my vision came back like a switch flipped. But yeah, the side effects? My face looked like a balloon for two months. Worth it though.
Sarah -Jane Vincent-19 January 2026
Let’s be real - uveitis isn’t random. Big Pharma pushes steroids because they’re cheap and profitable. Meanwhile, the real causes - mold exposure, Lyme disease, glyphosate in your food - are buried. Your doctor won’t test for it because insurance won’t pay. I had five flare-ups before someone finally checked my Lyme titers. Turns out I had it for years. Steroids masked it. The system is designed to keep you dependent, not cured.
Anna Hunger-20 January 2026
Thank you for this comprehensive and clinically accurate overview. As a healthcare professional, I appreciate the clear delineation between uveitis types and the corresponding therapeutic approaches. It is imperative that patients understand the distinction between anterior and posterior involvement, as prognosis and management differ significantly. Early referral to a uveitis specialist remains the gold standard, and patient education regarding the risks of delayed treatment cannot be overstated.
Jason Yan-21 January 2026
It’s wild how the body fights itself sometimes. Like your immune system’s got a grudge against your eyeball and won’t let go. I used to think inflammation was just swelling, but this? It’s like your eye’s in a civil war and your own cells are the enemy. Steroids are the ceasefire - they don’t fix the reason the war started, but they stop the bullets flying. That’s why I think we need to stop seeing uveitis as ‘an eye problem’ and start seeing it as a signal - your body’s screaming that something’s off, deep down. Maybe it’s stress. Maybe it’s gut health. Maybe it’s something we haven’t figured out yet. But ignoring it? That’s like ignoring a smoke alarm because the fire hasn’t burned your house yet.
shiv singh-22 January 2026
You people are so naive. They tell you it’s ‘idiopathic’ but they know. They always know. The government hides the truth because if people knew uveitis was linked to 5G and vaccines, they’d riot. I know a guy who got it after his flu shot. He lost 70% of his vision. The doctors gave him steroids and told him to ‘stay positive.’ Meanwhile, the real cause? Chemical weapons testing in the water supply. I’ve been researching this for 8 years. You think your eye doctor cares? No. They’re paid to keep you on drugs. I went natural - turmeric, cold laser, and a strict no-sugar diet. My uveitis vanished in 11 weeks. They don’t want you to know this.
Robert Way-24 January 2026
Just had my first flare-up last week. Got the drops. But I’m scared to use them too long. My friend said her eye pressure went nuts and now she’s got glaucoma. I’m gonna ask my doc about that methotrexate thing you mentioned. I don’t wanna be on steroids forever. Just wanna see my kid’s face clearly.