Running out of your blood pressure or cholesterol meds shouldn’t feel like a crisis. Yet for millions of people taking daily generic medications, remembering to refill prescriptions is a constant mental load. That’s where automated refills come in - a simple, quiet innovation that’s quietly improving how people manage chronic conditions. No more last-minute pharmacy runs, no more missed doses because you forgot to call. Just your meds showing up on time, every time.
How Automated Refills Actually Work
Automated refill systems don’t magic up your pills. They’re smart reminders built into your pharmacy’s system. When you’re prescribed a long-term generic medication - say, metformin for diabetes or lisinopril for high blood pressure - the pharmacy tracks your supply. Most systems trigger a refill request about 5 to 7 days before you run out. That’s not random. It’s based on how long it takes for the med to be processed, shipped, and delivered. If you’re using a mail-order pharmacy, your pills might arrive right before your current bottle empties. If you pick up in-store, you’ll get a text or email saying your refill is ready. It’s not automatic in the sense that the pharmacy just sends more without asking. You have to opt in. That means signing up through your pharmacy’s website, app, or in person. Once enrolled, the system will keep refilling your prescription on schedule unless you tell them to stop. Some systems even let you adjust the timing - like switching from a 30-day to a 90-day supply if your doctor approves it. This isn’t just a convenience feature. It’s backed by data. A 2016 study of Medicare Part D users found that people on automated refills had 7.2% higher adherence for statins, 3.9% higher for blood pressure meds, and 6.8% higher for diabetes drugs compared to those who had to request refills manually. That’s not a small number. It’s the difference between staying healthy and ending up in the hospital.Why Generic Medicines Are the Perfect Fit
Automated refills work best with generic medications - and for good reason. Generics are the backbone of long-term treatment. They’re cheaper, widely available, and prescribed for conditions that require daily, uninterrupted use. Think thyroid meds, antidepressants, statins, and antihypertensives. These aren’t drugs you take for a week. They’re lifestyle anchors. Because generics are so common and consistent in quality, pharmacies can standardize refill cycles without worrying about brand-specific dosing quirks or supply shortages. That makes automation smooth and reliable. You’re not getting a different version of the drug each time. The same generic manufacturer’s product arrives every cycle, so your body isn’t adjusting to new fillers or coatings. Also, most insurance plans and Medicare Part D plans heavily favor generics. That means lower copays and fewer out-of-pocket surprises. When you combine low cost with automated refills, you remove two big barriers to adherence: cost and effort. It’s no surprise that 48% of commercially insured patients in the U.S. are now enrolled in some form of automated refill program.The Real Benefits: More Than Just Convenience
Sure, not having to remember to call the pharmacy is nice. But the real win is what happens when you stop missing doses. People on automated refills have fewer ER visits. Fewer hospitalizations. Fewer complications. For someone with heart disease or diabetes, that’s life-changing. Pharmacies see it too. Clarity Ventures reported a 37% drop in manual refill follow-up calls after implementing automated systems. That means pharmacy staff spend less time chasing down patients and more time helping people with questions, checking for drug interactions, or counseling on side effects. It’s not just about efficiency - it’s about better care. For older adults or people with memory issues, automated refills are a lifeline. One study found patients with cognitive challenges maintained over 95% adherence rates when using automated systems. Without it, they were missing doses 30% of the time. Even the financial side adds up. The Centers for Medicare & Medicaid Services (CMS) now rate plans based on how well patients take their meds. Plans with higher adherence scores get bonus payments - around $127 per member per year. That’s why nearly two-thirds of Medicare Part D plans now offer automated refills. It’s good for patients. It’s good for the system.Where Things Can Go Wrong
Nothing’s perfect. The biggest risk with automated refills? Dosage changes. Let’s say your doctor increases your diltiazem from 240 mg to 360 mg because your blood pressure isn’t controlled. If you’re on auto-refill, and your pharmacy doesn’t catch the update in your electronic record, you’ll keep getting the old dose. That’s not just inconvenient - it’s dangerous. Consumer Medication Safety documented several cases like this in late 2024. In one, a patient kept receiving 240 mg of diltiazem for three months after their doctor changed the prescription. The patient didn’t notice because the pills looked the same. They only found out during a routine checkup. That’s why you need to stay involved. Always confirm dosage changes with your pharmacy. If your doctor updates your script, call the pharmacy and say, “I need to make sure my auto-refill reflects this new dose.” Don’t assume they’ll catch it. Most systems are smart, but they’re not mind readers. Another issue? Unexpected deliveries. Some people don’t realize they’ve been enrolled. You might get a box of pills you didn’t order, and suddenly you’re paying out of pocket for meds you thought you’d stopped. That happened to 31% of negative reviews on One Medical’s Trustpilot page in early 2024. Always check your enrollment status. If you don’t want auto-refills, turn them off.Amazon RxPass and Other New Models
The landscape is changing fast. Amazon Pharmacy launched RxPass in January 2023 - a flat $5 monthly fee for 60 common generic medications for Prime members in 45 states. No copays. No insurance hassle. Just pick your meds, pay $5, and get them delivered with auto-refills built in. JAMA Network Open reported that RxPass users increased their refill rates by 18% in the first year. Why? Because the barrier to getting meds was gone. No more fighting with insurance, no more $40 copays for metformin. For people on tight budgets, this is huge. Other big players are catching on. CVS Health integrated its auto-refill system with Apple Health in late 2023. Now your medication schedule shows up in your iPhone’s Health app. You can see when your next refill is due, track adherence over time, and even get reminders synced with your calendar. These aren’t gimmicks. They’re the future. And they’re built on one simple idea: if you make it easier to take your meds, people will take them.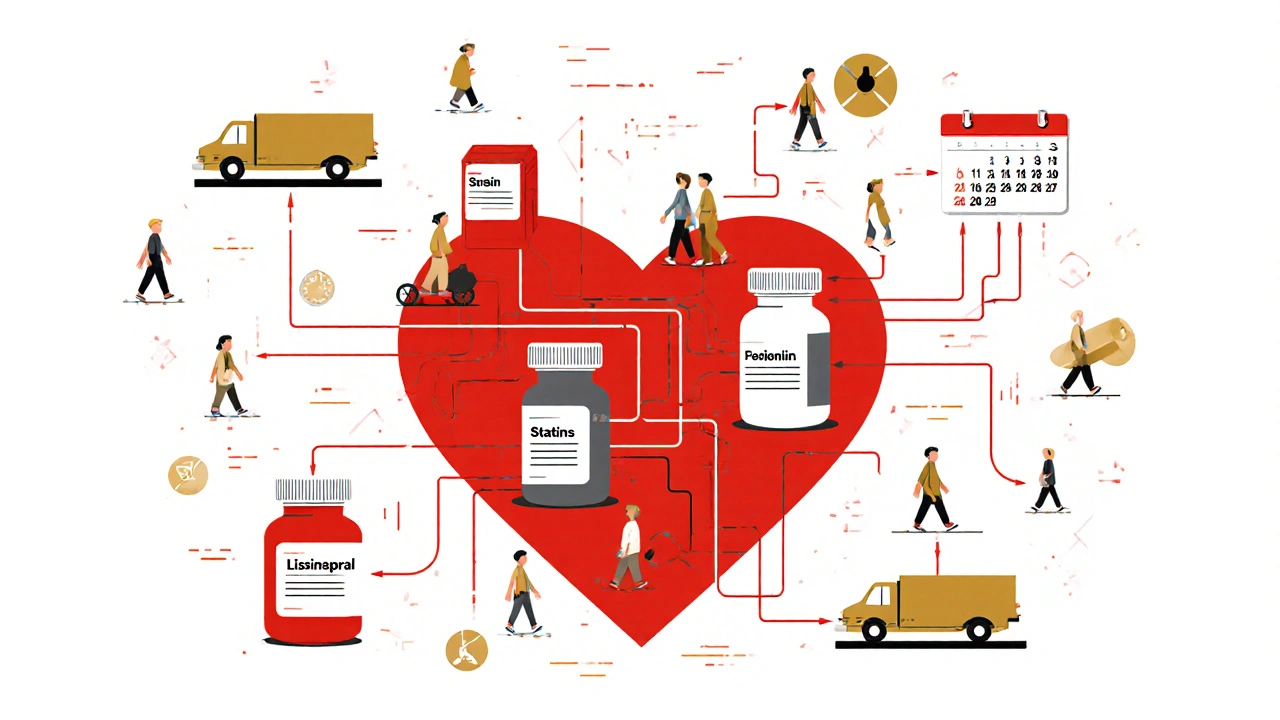
How to Get Started
Signing up is easy, but you have to take the first step.- Log into your pharmacy’s website or app (CVS, Walgreens, Walmart, or your local chain).
- Find the “Refill Settings” or “Auto-Refill” section.
- Select the medications you want on auto-refill - usually only chronic condition drugs.
- Choose your refill schedule: 30-day or 90-day supply.
- Confirm your delivery method: pick up in-store or home delivery.
- Accept the terms - you’ll need to give consent, since it’s a HIPAA-protected service.
What Experts Say - And Why It Matters
Dr. CA Lester’s 2016 study was one of the first to prove automated refills improve adherence. He didn’t just look at numbers - he looked at real people. His team found no increase in medication waste. In fact, oversupply dropped because people were getting the right amount at the right time. The American Medical Association backs this up. Their Steps Forward module says automated refills reduce interruptions for doctors, cut down on pharmacy follow-up calls, and make patients happier. When patients aren’t worried about running out, they feel more in control. But not everyone’s convinced. KevinMD, a popular physician blog, argued in 2022 that auto-refills are more about profit than patient care. Some pharmacy benefit managers (PBMs), they say, set refill triggers at 60 days into a 90-day script to boost revenue. That means you get a refill before you need it - and pay more in shipping or copays. That’s a real concern. But it’s not a flaw in auto-refills themselves. It’s a flaw in how some companies run them. The solution? Know your plan. Check your refill schedule. If you’re getting meds every 60 days but your doctor prescribed a 90-day supply, ask why. You have the right to choose.Final Thoughts: It’s Not About Technology - It’s About Care
Automated refills aren’t flashy. No one posts about them on TikTok. But for the millions managing high blood pressure, diabetes, or depression, they’re the quiet hero of daily health. They don’t cure anything. But they make it possible to stick with treatment - day after day, month after month. The tech is good. The data is solid. The savings are real. But the biggest benefit? Peace of mind. Knowing your meds are on the way means you can focus on living - not remembering to call the pharmacy. If you’re on a daily generic medication, ask your pharmacy about auto-refills today. It takes minutes. And it could change how you feel - every single day.Are automated refills safe for all medications?
Automated refills work best for chronic, daily medications like blood pressure pills, statins, or diabetes drugs. They’re not recommended for antibiotics, pain meds, or drugs with frequent dosage changes. Always check with your pharmacist before enrolling in auto-refill for any new medication.
Can I change my refill schedule after signing up?
Yes. Most pharmacy apps and websites let you adjust your refill frequency - from 30-day to 90-day supplies - or pause auto-refills temporarily. You can also remove a medication from the list entirely. Just log in and update your preferences, or call the pharmacy directly.
Do I need insurance to use automated refills?
No. While insurance helps lower your cost, you can still use auto-refill services without it. Pharmacies like Walmart and CVS offer low-cost generic programs. Amazon RxPass also lets you pay a flat $5 monthly fee for 60 common generics - no insurance needed.
What if I stop taking a medication? Will it still be refilled?
Yes - unless you remove it from your auto-refill list. Pharmacies rely on electronic prescriptions, not your word. If your doctor stops your script, the system may still auto-refill if the prescription hasn’t been canceled. Always notify your pharmacy if you’re discontinuing a drug, even if you think your doctor already did.
Are automated refills available in Australia?
Currently, automated refill systems like those in the U.S. are not widely available in Australia. Most Australian pharmacies still require patients to request refills manually. However, some private online pharmacies and telehealth providers are testing similar systems. Check with your local pharmacy or use apps like HealthEngine or MedAdvisor to set refill reminders - they’re not automatic, but they help you stay on track.




11 Comments
Anne Nylander-21 November 2025
Just signed up for auto-refill on my metformin yesterday-life changed. No more panic at 11pm when I realize I’m out. I actually slept through the night. 🙌
Franck Emma-22 November 2025
I hate this. My box showed up two days before I needed it. Now I have to store extra pills. And I didn’t even ask for it. This isn’t convenience-it’s corporate overreach.
Daisy L-23 November 2025
OMG YES!! I’ve been on lisinopril for 12 years and I used to forget EVERY. SINGLE. TIME. Now? My meds show up like magic. America’s greatest innovation since sliced bread-and it’s FREE with insurance!! 🇺🇸💥
Noah Fitzsimmons-25 November 2025
Of course you love it. You didn’t even read the part about how pharmacies auto-refill you at 60 days on a 90-day script just to squeeze more copays out of you. You’re not empowered-you’re being monetized. 🤡
Eliza Oakes-26 November 2025
Wait-so you’re telling me this isn’t just a scheme to get people addicted to their meds? Like, what if I want to stop? What if I’m trying to heal naturally? This feels like pharmaceutical control disguised as care.
Corra Hathaway-26 November 2025
Y’all are overthinking this. I’ve got 3 meds on auto-refill and my mom (78, dementia) hasn’t missed a dose in 14 months. That’s not corporate greed-that’s dignity. 🤗 If you’re scared of convenience, maybe you’re not ready for adulthood.
Leo Tamisch-26 November 2025
One must ask: is the automation of pharmaceutical adherence a symptom of our alienation from bodily autonomy, or merely a pragmatic solution to a systemic failure of human memory? The pills arrive on schedule-but do we still own our healing? The algorithm knows when we’ll run out. But does it know why we began taking them? 🤔
Shawn Sakura-27 November 2025
Just wanted to say-this system saved my life. I’m diabetic, work two jobs, and forget everything. Auto-refill means I don’t have to choose between rent and meds. Thank you to whoever built this. 🙏 (Sorry for typos-typing on phone at 3am after shift)
Paula Jane Butterfield-28 November 2025
For those in rural areas or without reliable internet-this is a game changer. My grandma in rural Kansas got her statins delivered every month without ever leaving her porch. Pharmacies should be required to offer this. Also, if you’re on Amazon RxPass-YES, it’s legit. $5/month for metformin? That’s a moral victory.
Donald Frantz-29 November 2025
What about drug interactions? The system doesn’t know if you started a new antibiotic or NSAID. I’ve seen patients get refilled statins while on grapefruit juice and a new beta-blocker. Automation without clinical oversight is dangerous. This isn’t a feature-it’s a liability waiting to happen.
Sammy Williams-30 November 2025
Just got my first auto-refill box today. Took me 5 minutes to sign up. My blood pressure meds are here. I’m not overthinking it. I’m just glad I don’t have to remember anymore. Thanks, internet.