Chronic pain isn't just a symptom-it's a whole new way of living.
When pain lasts longer than three months, it stops being a warning sign and becomes a condition of its own. Millions of people wake up every day not because they’re ready to start their day, but because they have to survive it. Chronic pain doesn’t go away with rest, ice, or even strong painkillers. It rewires your nervous system, steals your sleep, drains your energy, and makes even simple tasks feel impossible. The goal isn’t to make the pain vanish-it’s to help you live well despite it.
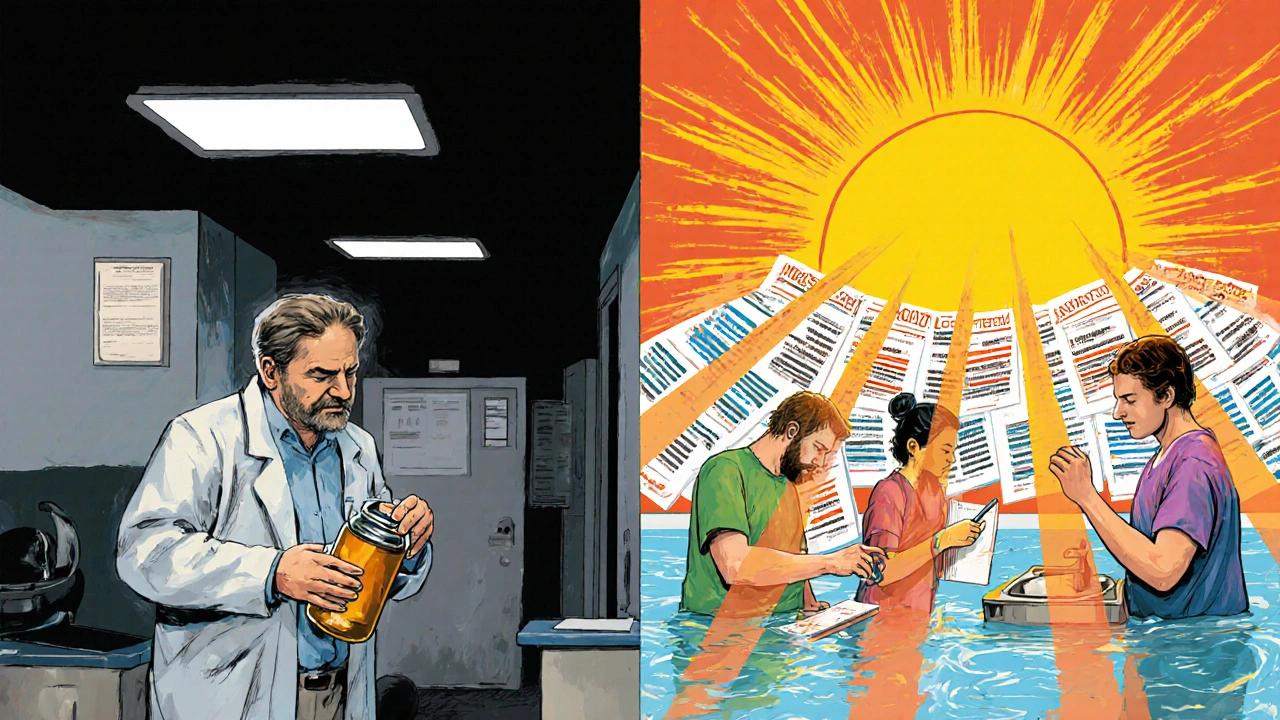
Why traditional pain treatments often fail
For years, the default answer to chronic pain was pills-especially opioids. But the reality is harsh: opioids work well for a few weeks, then their power fades. By six months, most people see little to no extra pain relief, yet the risks keep climbing. The CDC found that people taking more than 50 morphine milligram equivalents (MME) per day are 40% more likely to overdose. And that’s not even counting the addiction, fatigue, constipation, and mental fog that come with long-term use.
Many patients report being offered only two choices: take stronger pills or deal with the pain alone. That’s not treatment-it’s neglect. Primary care doctors, often under time pressure and lacking specialized training, aren’t equipped to offer better alternatives. A 2022 study showed only 35% of them had received proper training in non-opioid pain management. So patients are left stuck, cycling through medications that don’t work long-term and feeling unheard.
The real solution: non-pharmacological approaches that work
The most effective treatments for chronic pain don’t come in a bottle. They come from movement, mindset, and mastery. The latest guidelines from the WHO, CDC, and American College of Physicians all agree: start with drug-free options.
- Structured exercise-not just walking, but tailored programs that include aerobic activity, strength training, yoga, tai chi, and water-based exercises. Studies show these reduce pain by 15-30% and improve daily function by 20-40% after 6-12 weeks of consistent effort.
- Cognitive Behavioral Therapy (CBT)-a proven psychological tool that helps you change how you respond to pain. After 8-12 weekly sessions, patients report 25-40% less pain intensity, 30% less disability, and up to 50% less catastrophizing (the spiral of thinking "this pain will destroy my life").
- Multidisciplinary rehabilitation-the gold standard. Programs like the one at Mayo Clinic bring together physical therapists, psychologists, pain specialists, and occupational therapists in a three-week intensive course. Participants learn to manage triggers, reduce stress, retrain movement patterns, and rebuild confidence. Sixty to seventy-five percent leave with meaningful improvements in function, and half reduce or stop opioids entirely.
These aren’t "alternative" treatments-they’re evidence-based, clinically proven, and endorsed by top medical organizations. Yet they’re rarely offered first. Why? Because they take time, require trained staff, and aren’t as profitable as prescriptions.
What about medications? When and how they fit
Medications still have a place-but only after non-drug options have been tried, and only when used carefully.
- Acetaminophen (up to 3,000-4,000 mg/day) is safe for many, but doesn’t work for everyone.
- NSAIDs like ibuprofen (1,200-3,200 mg/day) or naproxen (500-1,000 mg/day) help with inflammation-related pain, but aren’t safe for long-term use in people with kidney or stomach issues.
- Co-analgesics like duloxetine (60-120 mg/day) and pregabalin (150-600 mg/day) target nerve pain and can be very effective for conditions like diabetic neuropathy or fibromyalgia.
- Opioids should be a last resort. If used, they must start at the lowest possible dose, never exceed 50 MME/day, and be reviewed monthly. They’re not for long-term daily use.
One key point: pain scores don’t tell the whole story. A patient might still feel pain at a level of 6/10-but if they can now cook dinner, play with their grandkids, or sleep through the night, that’s progress. The goal isn’t zero pain. It’s a life worth living.
Why access is the biggest barrier
Even the best treatments won’t help if you can’t get them.
- Cost: A full multidisciplinary rehab program can cost $15,000-$20,000. Most insurance plans cover only a fraction-or none at all.
- Location: Only 15-20% of eligible patients can access these specialized programs because they’re mostly in big cities. In rural areas, 65% of counties have no pain specialist at all.
- Insurance denials: Even when guidelines say CBT or physical therapy should be first-line, insurers often deny coverage, calling them "experimental" or "not medically necessary."
- Provider gaps: A 2023 survey found 68% of patients couldn’t find a provider trained in non-opioid pain management. One Reddit user summed it up: "My doctor only offered opioids or nothing."
There’s a stark contrast between what works and what’s available. Patients who complete rehab programs report 85% satisfaction rates. Yet most never even get the chance.
What’s changing-and what’s not
The tide is turning, slowly.
- The CDC updated its opioid guidelines in 2022, pushing hard for non-drug treatments.
- Medicare expanded coverage for physical therapy, CBT, and acupuncture in 2023.
- The VA now offers multidisciplinary pain programs in 92% of its facilities-far ahead of civilian hospitals, where only 22% do.
- New digital tools are emerging: FDA-cleared apps like reSET-O and wearable neuromodulation devices (like Nevro’s Senza) show 30-40% pain reduction in trials.
But progress is uneven. Black patients are 40% less likely to receive recommended non-drug treatments, even when their pain levels are the same as white patients. Rural communities still have no access. Clinicians are overwhelmed by paperwork-CDC guidelines require detailed progress notes, urine screens, and risk assessments, which many practices can’t handle.
The NIH has invested $1.8 billion into developing non-addictive pain treatments, with 12 new drugs in late-stage trials. But innovation won’t help if the system doesn’t change.

How to start managing your chronic pain today
You don’t need to wait for the system to fix itself. Here’s how to take control, even with limited resources:
- Track your pain: Use the Brief Pain Inventory (BPI) or a simple journal. Note what makes it better or worse-not just the number, but the context.
- Move daily: Start with 10 minutes of walking, swimming, or seated stretches. Consistency beats intensity. Aim for 3-4 days a week.
- Find free CBT resources: Apps like MoodGYM or online programs from the American Chronic Pain Association offer structured CBT modules at no cost.
- Ask for referrals: Request a physical therapist, psychologist, or pain specialist. If your doctor says no, ask why-and request a written explanation.
- Connect with others: Online communities like r/ChronicPain can offer emotional support and practical tips. You’re not alone.
Progress isn’t linear. Some days will feel like setbacks. But small, steady actions build real change. One veteran shared: "After 12 sessions of CBT, I went from 120 MME/day to 30 MME/day-and actually started playing with my kids again."
What’s next for chronic pain care
The future lies in integration. Pain management must become part of routine care-not a last-ditch effort. Primary care clinics need embedded pain specialists. Insurance must cover evidence-based therapies without endless paperwork. Medical schools must teach the biopsychosocial model: pain isn’t just in the body, it’s shaped by emotions, stress, sleep, and social support.
Dr. Sean Mackey of Stanford says it best: "Effective chronic pain management requires addressing the biological, psychological, and social dimensions of pain simultaneously." That’s not a slogan-it’s the science.
The path forward isn’t about finding a miracle cure. It’s about rebuilding a life that pain can’t steal. And that’s possible-every day, for millions, it already is.
Is chronic pain curable?
Chronic pain is rarely "cured" in the traditional sense, especially when it stems from nerve damage, arthritis, or long-term changes in the nervous system. But it can be effectively managed. Many people learn to reduce pain intensity, regain function, and return to meaningful activities-even if some discomfort remains. The goal isn’t to eliminate pain entirely, but to restore quality of life.
Can I stop taking opioids safely?
Yes, but it must be done carefully and with support. Stopping opioids abruptly can cause withdrawal symptoms like nausea, anxiety, and increased pain sensitivity. Work with a pain specialist or addiction medicine provider to create a tapering plan-usually over weeks or months. Pair this with non-opioid treatments like CBT or physical therapy. Studies show people who taper with support often experience improved function and reduced side effects, even if pain doesn’t disappear completely.
Does insurance cover non-drug pain treatments?
Coverage varies widely. Medicare now covers CBT, physical therapy, and acupuncture for chronic pain. Private insurers are slower to adapt, and many still deny claims for these services, labeling them "experimental." Always ask for a written denial and appeal. Some states have laws requiring coverage for certain therapies. The American Chronic Pain Association offers free templates to help you appeal insurance denials.
What’s the best exercise for chronic pain?
There’s no single "best" exercise-it’s about what you can do consistently. Walking, swimming, cycling, yoga, and tai chi are all excellent because they’re low-impact and improve mobility. Strength training helps stabilize joints and reduce strain. The key is starting slow and building gradually. A physical therapist can tailor a program to your specific condition. Studies show programs lasting 6-12 weeks, done 2-3 times per week, produce the strongest results.
How do I find a pain specialist?
Start by asking your primary doctor for a referral to a pain management clinic that uses a multidisciplinary approach. Look for clinics affiliated with academic hospitals or the VA system-they’re more likely to follow evidence-based guidelines. You can also search through the American Academy of Pain Medicine or the American Chronic Pain Association’s provider directories. Avoid clinics that rely heavily on injections or opioids without offering physical or psychological therapies.
Are there free or low-cost resources for chronic pain?
Yes. The American Chronic Pain Association offers free educational materials and peer support groups. Apps like PainScale and Mindfulness Coach help track pain and practice relaxation. YouTube has guided yoga and tai chi videos designed for chronic pain. Local libraries and community centers sometimes offer free or low-cost physical therapy classes. The NIH’s HEAL Initiative also provides free online resources for patients and caregivers.
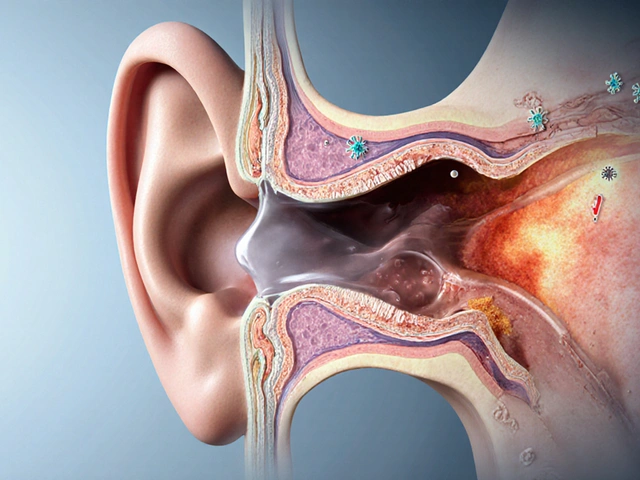
Why does stress make my pain worse?
Stress activates your nervous system, which can heighten pain signals. When you’re stressed, your body releases hormones like cortisol and adrenaline that make nerves more sensitive. This is called central sensitization-it’s why pain feels sharper and spreads to new areas under stress. Techniques like deep breathing, CBT, and mindfulness help calm the nervous system. Many patients report that managing stress reduces their pain intensity even without changing their physical condition.
Can chronic pain affect my mental health?
Absolutely. Chronic pain and mental health are deeply linked. Up to 80% of people with chronic pain also experience depression, anxiety, or sleep disorders. This isn’t "all in your head"-it’s a biological reality. Constant pain wears down your brain’s ability to regulate mood and stress. That’s why CBT and other psychological therapies are core parts of treatment. Addressing mental health isn’t optional-it’s essential to managing pain effectively.
Final thoughts: You’re not broken-you’re adapting
Living with chronic pain doesn’t mean you’ve failed. It means you’re surviving a system that wasn’t built for you. The real victory isn’t in erasing pain-it’s in reclaiming your life despite it. Whether it’s cooking a meal, playing with your dog, or sleeping through the night, those moments matter. Progress is messy. Some days you’ll feel strong. Others, you’ll just get through. That’s okay. You’re not chasing a cure. You’re building resilience. And that’s something no pill can give you.




9 Comments
Lisa Detanna-23 November 2025
After years of being told to just 'push through' or 'take more pills,' I finally found a pain clinic that actually listened. CBT and water aerobics twice a week changed everything. I can now hold my granddaughter without crying. No magic cure, but damn if it isn't progress.
And yeah, insurance denied it twice. I appealed. They finally approved after I sent them the CDC guidelines printed out. Sometimes you gotta fight the system to get the care you deserve.
Demi-Louise Brown-23 November 2025
Effective chronic pain management requires consistency, not intensity. Small daily actions compound into meaningful change. Movement, mindfulness, and structured routines are not luxuries-they are medical necessities.
Insurance barriers and provider gaps are systemic failures, but individual agency remains. Start with one minute of stretching. Then ten. Then thirty. Progress is not linear, but it is possible.
Ragini Sharma-24 November 2025
bro i tried yoga for like 3 days and my back felt worse so i gave up lmao guess im just doomed to be on vicodin forever
Manjistha Roy-26 November 2025
It's not enough to say 'non-pharmacological approaches work'-we need to demand that they be accessible, affordable, and covered without endless paperwork. The fact that a veteran can reduce opioids from 120 MME to 30 MME and play with their kids again? That's not anecdotal-it's evidence.
And yet, in rural areas, there are no specialists. In low-income communities, the programs are priced out of reach. This isn't a medical issue-it's a moral one.
We need policy change, not just personal resilience.
JD Mette-28 November 2025
I appreciate the depth of this post. It's rare to see such a balanced view that doesn't villainize medication or dismiss non-drug options.
I've been managing neuropathic pain for eight years. The CBT helped me reframe my relationship with pain, but it didn't erase it. And that's okay. What matters is that I can still work, still laugh, still be present.
Thank you for acknowledging that progress isn't about zero pain-it's about a life worth living.
Olanrewaju Jeph-30 November 2025
It is imperative to note that cultural context significantly influences pain perception and treatment adherence. In many African communities, pain is often endured silently due to stigma or lack of access, yet the principles of movement, mindfulness, and multidisciplinary care remain universally applicable.
For those without insurance, community-based peer groups and free online resources-such as those from the NIH HEAL Initiative-are invaluable. Consistency, not perfection, is the cornerstone of sustainable management.
Dalton Adams-30 November 2025
Let me just say this: if you're still relying on acetaminophen or NSAIDs for chronic pain, you're doing it wrong. 🤦♂️
Real pain management isn't about walking or yoga-it's about neuromodulation devices, precision medicine, and functional MRI-guided interventions. The fact that most people haven't even heard of Nevro's Senza? That's not a gap in care-that's a failure of the entire medical education system.
And don't get me started on CBT. It's not a cure. It's a band-aid for people who can't afford real tech. The VA does it right because they have the budget. Your primary care doc? They're still using 1998 protocols.
Stop romanticizing 'movement' and start demanding innovation. The future is wearable neurotech, not seated stretches.
Also, if you're using YouTube yoga videos, you're probably making your condition worse. 😅
Kane Ren-30 November 2025
I used to think I was broken because I couldn't just 'get over it.'
Then I found a physical therapist who didn't push me to lift heavy weights on day one. She met me where I was. We started with breathing exercises and 5-minute walks. Now, I can carry groceries. I can sleep without waking up screaming.
It wasn't fast. It wasn't glamorous. But it was real.
You're not failing. You're adapting. And that's more courageous than any pill.
Charmaine Barcelon- 2 December 2025
If you're not doing daily stretching, meditation, and tracking your pain in a journal, you're just wasting time. Why are people still on opioids? It's lazy. It's irresponsible. You have to WANT to get better.
And if your doctor won't refer you? Fire them. There are tons of pain specialists out there-you just have to be proactive. No one is going to save you. You have to save yourself.
And stop blaming insurance. That's not the problem. The problem is you're not trying hard enough.