Why so many people still think generic drugs don’t work
You walk into the pharmacy to pick up your prescription. The pharmacist hands you a small white pill in a plain bottle. "This is the generic version of your brand-name drug," they say. You look at it. It doesn’t look like the one you’ve been taking. The color is different. The shape is weird. The label doesn’t say the name you recognize. You hesitate. "Is this really the same?"
You’re not alone. Nearly 4 in 10 Americans still believe generic drugs are less effective than brand-name ones-even though the FDA says they’re required to work the same way. This isn’t about science. It’s about language. And how we explain it.
What a generic drug actually is (no jargon)
A generic drug is not a copy. It’s not a knockoff. It’s not a cheaper version that got approved because no one was looking. It’s the exact same medicine, legally required to be identical in one critical way: the active ingredient.
Let’s break that down. If your brand-name drug is Lipitor (atorvastatin), the generic is just atorvastatin. Same chemical. Same strength. Same way it works in your body to lower cholesterol. The FDA doesn’t approve a generic unless it delivers the same amount of medicine into your bloodstream as the brand-within a tiny, scientifically proven range of 80% to 125%. That’s not a guess. That’s a rule.
What’s different? The color. The shape. The filler inside the pill (like lactose or cornstarch). The brand name on the bottle. But none of that changes how the medicine works. Think of it like buying store-brand cereal. Same ingredients. Same nutrition. Different box. Same bowl.
How language guides fix the confusion
For years, patients got brochures written by scientists-for other scientists. Words like "bioequivalence," "pharmacokinetics," and "therapeutic index" made people feel stupid. And confused.
Now, smarter tools are being used. Consumer language guides cut the fluff. They use real analogies. "Tylenol is to acetaminophen what Kleenex is to tissues." Simple. Familiar. Easy to remember.
Pharmacies like CVS, Walgreens, and Walmart now train their staff to explain generics in 90 seconds using three clear points:
- Same active ingredient-the part that does the work.
- Same effect-FDA requires it to work just as well.
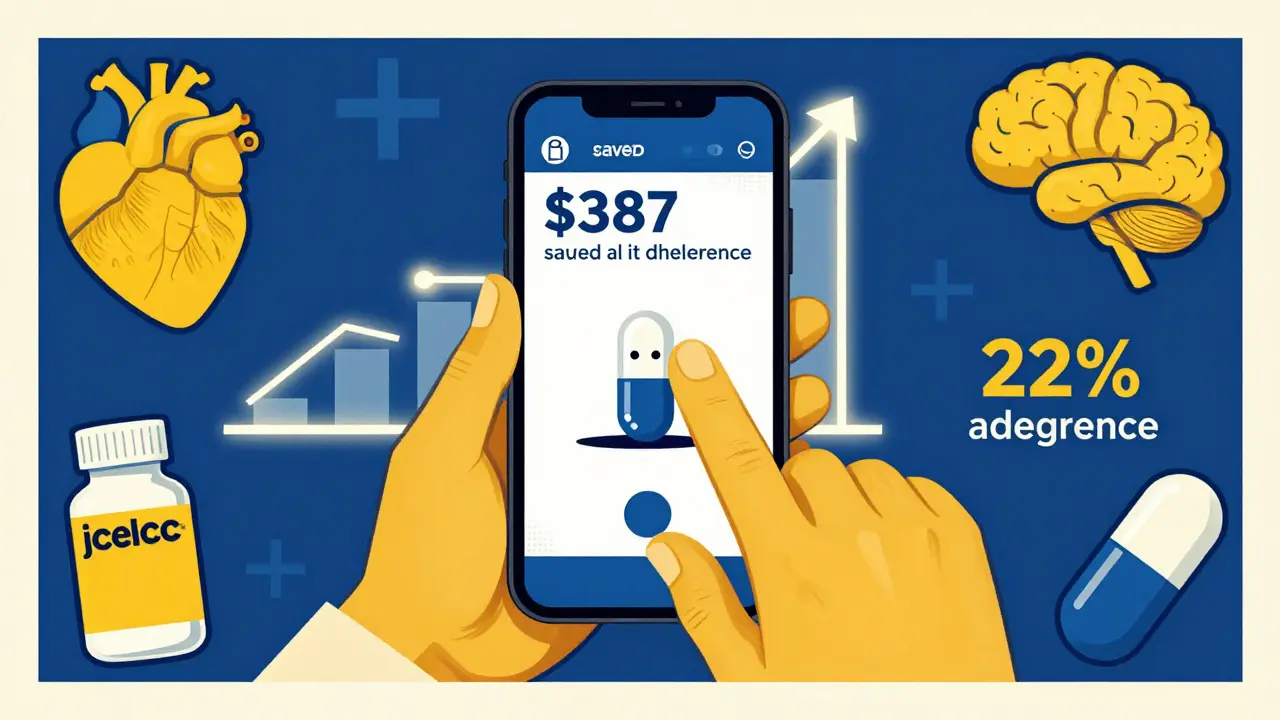
- Same cost savings-on average, $387 less per prescription.
They also use side-by-side pictures. One photo shows the brand-name pill. The next shows the generic. Same size. Same shape. Different color. No magic. Just science.
When generics aren’t exactly the same (and why that matters)
Here’s the hard truth: most generics are identical. But not all.
Some medicines need to be *extremely* precise. Think thyroid meds like levothyroxine or seizure drugs like phenytoin. Tiny changes in how the body absorbs the drug can make a big difference. That’s why some doctors still recommend sticking with one brand-or one generic manufacturer-for these drugs.
The FDA knows this. That’s why they don’t say "all generics are the same." They say "generics must be equivalent." There’s a difference. Good language guides don’t overpromise. They say: "For most drugs, generics work just fine. For a few, your doctor might suggest sticking with one version. Ask them if yours is one of those."
And then there’s the authorized generic. This is the brand-name drug-made by the same company-but sold under a generic label. No fancy packaging. Same pill. Same price as a regular generic. These have the lowest switch-back rates. And most patients don’t even know they exist.
What the data really says
Let’s look at what happens when people actually understand generics.
A study of 12 million patients found that when pharmacists used plain language to explain generics, patients stuck with them 22% longer. They switched back to expensive brand names 34% less often.
And the savings? Huge. In 2022, generics made up 90.9% of all prescriptions filled in the U.S.-but only 22.3% of total drug spending. That’s because generics cost way less. The average savings per prescription? $387. Multiply that by billions of prescriptions, and you’re talking about billions saved every year.
Meanwhile, confusion costs money. The Association for Accessible Medicines estimates that because people don’t trust generics, the system spends an extra $3.2 billion a year on unnecessary brand-name prescriptions.
What works-and what doesn’t-in patient education
Not all guides are created equal.
The FDA’s "Generic Drug Facts" page scores 87 out of 100 on health literacy tools. That’s excellent. Many pharmacy-made guides? Only 62. Why? Too much text. Too many big words. No visuals. No clear takeaway.
Good guides follow simple rules:
- Use short sentences. No more than 15 words.
- Use active voice: "Take this pill once a day" not "This pill should be taken once a day."
- Use real examples: "Nexium is the brand. Esomeprazole is the generic. Same medicine. Different name."
- Include a "teach-back" question: "Can you tell me in your own words why this generic will work just like your old pill?"
The best ones also show the chemical name. Not to impress you. But to prove it’s the same. N-(4-hydroxyphenyl) acetamide is the science name for acetaminophen, which is the generic name for Tylenol. Same thing. Just three ways to say it.
What’s changing right now
This isn’t static. The system is getting smarter.
In 2023, the FDA launched a $4.7 million initiative to build custom guides for tricky drugs like levothyroxine and warfarin. Medicare Part D plans must now offer plain-language materials that meet NIH health literacy standards by January 2025.
And the next step? Personalization. Pilot programs at Kaiser Permanente are testing AI tools that adjust explanations based on your literacy level, your age, and even your medication history. Imagine opening your pharmacy app and seeing a short video that says: "Your levothyroxine is a generic. Some people do better sticking with one brand. Would you like to talk to your doctor about it?"
By 2026, 60% of generic education will likely come from your electronic health record-right when you’re prescribed the drug. No more waiting for a brochure. No more forgetting what the pharmacist said.
What you can do today
You don’t need to wait for the system to catch up. Here’s what you can do right now:
- Ask your pharmacist: "Is this generic the same as my brand?" Then ask: "Are there any drugs where I should stick with one version?"
- Check the FDA’s "Generic Drugs" page. It’s free. No login. Updated every quarter.
- Look at the pill. Compare it to the brand. Same shape? Same size? Different color? That’s normal.
- Don’t assume a higher price means better quality. For generics, it doesn’t.
- If you feel different on a new generic, talk to your doctor. It might be the filler. It might be your body adjusting. But don’t assume it’s broken.
Final thought: Trust the science, not the label
Generic drugs saved the U.S. healthcare system nearly $2 trillion between 2009 and 2019. That’s not a marketing claim. That’s real money. Real people. Real health.
They’re not perfect. But they’re not magic either. They’re medicine-made to work. And the only thing standing between you and the savings is a misunderstanding.
Next time you see a plain bottle, remember: it’s not a downgrade. It’s the same medicine. Just without the brand name.
Are generic drugs really as effective as brand-name drugs?
Yes, for most medications. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also deliver the same amount of medicine into your bloodstream-within a scientifically proven range of 80% to 125%. Over 98% of approved generics meet this standard. The only difference is the inactive ingredients (like color or filler), which don’t affect how the drug works.
Why do generic pills look different from brand-name pills?
By law, generic drugs can’t look exactly like the brand-name version. That’s to avoid trademark infringement. So they change the color, shape, or size. But the active ingredient-the part that treats your condition-is identical. Think of it like two different brands of aspirin: one is red and oval, the other is white and round. They both contain acetylsalicylic acid. They work the same way.
Can I switch between different generic versions of the same drug?
For most drugs, yes. But for a small group called "narrow therapeutic index" drugs-like levothyroxine, warfarin, or phenytoin-switching between different generic manufacturers can sometimes cause issues. These drugs need to be absorbed very precisely. If you’re on one of these, your doctor might recommend sticking with the same generic brand. Always ask your pharmacist or doctor if your medication falls into this category.
What’s an authorized generic?
An authorized generic is the exact same drug as the brand-name version, but sold under a generic label and without the brand name on the packaging. It’s made by the same company that makes the brand, just at a lower price. These have the lowest rates of patients switching back to the brand-28% lower than regular generics-because they’re identical in every way, including the look and feel.
Why do some people say generics don’t work for them?
Sometimes, it’s psychological-people expect a change because the pill looks different. Other times, it’s because they switched between different generic manufacturers for a narrow therapeutic index drug. Rarely, a generic might have a manufacturing issue (like the 2012 case with a generic version of Wellbutrin XL). But these are exceptions. If you feel worse on a generic, talk to your doctor. Don’t assume it’s the drug-it might be your body adjusting, or you might need to stick with one brand.
Where can I find reliable information about my generic drug?
Start with the FDA’s "Generic Drugs" webpage, updated quarterly. It includes side-by-side comparisons, explanations of bioequivalence, and lists of authorized generics. Your pharmacist can also show you printed materials from the FDA or the Academy of Managed Care Pharmacy. Avoid relying on marketing sites or social media rumors-stick to official sources.



15 Comments
Prajwal Manjunath Shanthappa- 2 February 2026
Oh, please. Let’s not pretend this is some revolutionary breakthrough in pharmaceutical communication. We’ve had plain-language guides since the 90s. The real issue? Pharma companies still profit from fear-mongering. And now, with AI-driven personalization, they’ll just weaponize it better. 😏
Wendy Lamb- 3 February 2026
Simple. Clear. Effective. I’ve used these exact phrases with my patients for years. No jargon. No panic. Just facts. If we can make this standard everywhere, we save lives-and money.
Antwonette Robinson- 5 February 2026
Oh wow. A whole article about telling people ‘it’s the same pill.’ Groundbreaking. Next up: ‘Water is wet.’ The real scandal? The FDA lets companies change fillers that cause real reactions-and calls it ‘equivalent.’
Ed Mackey- 5 February 2026
Good stuff. I didn’t know about authorized generics. That’s actually kinda cool. I always thought generics were just knockoffs. My bad. 🤷♂️
Katherine Urbahn- 6 February 2026
While the intent of this article is commendable, its underlying assumption-that consumer comprehension is the primary barrier to generic adoption-is dangerously reductive. The systemic disincentives embedded within insurance formularies and physician prescribing habits remain unaddressed. One cannot remedy institutional failure with a pamphlet.
Alex LaVey- 6 February 2026
I’m from the Midwest, and I’ve seen this work. People don’t trust what they don’t understand. But when you show them the pill side-by-side and say, ‘Same stuff, different box,’ they get it. No magic. Just honesty. That’s all we need.
Justin Fauth- 7 February 2026
They’re trying to trick us. Generic drugs? Nah. They’re using cheaper fillers that mess with your gut. I switched to one and got dizzy for a week. They don’t tell you that. The FDA’s just in bed with Big Pharma. Wake up, sheeple!
Meenal Khurana- 7 February 2026
My mom switched to generic blood pressure meds. No issues. Saved $200/month. Simple.
Joy Johnston- 7 February 2026
Let’s not overlook the critical role of pharmacist counseling. The 22% increase in adherence isn’t just from brochures-it’s from trained staff taking 90 seconds to say, ‘This is the same medicine. Here’s why.’ That’s human connection. That’s healthcare.
Shelby Price- 8 February 2026
So… the pill looks different but does the same thing? Huh. 😅 I always thought the color meant something. Guess I’ve been overthinking it.
Jesse Naidoo-10 February 2026
Wait-so you’re telling me the company that made my brand drug also makes the generic? And I didn’t know that? That’s insane. Why didn’t anyone tell me? This feels like a scam.
Sherman Lee-12 February 2026
They’re testing AI on your EHR? 🤖 Next thing you know, your phone will tell you what pill to take before you even see a doctor. Welcome to the dystopia, folks. The government’s not helping you-they’re automating your compliance. 💀
Lorena Druetta-12 February 2026
This is so important. I work in a clinic where people skip meds because they think generics are ‘inferior.’ One woman cried when she realized her heart pill was the same-she’d been paying $150 a month for nothing. Thank you for saying this out loud.
Zachary French-14 February 2026
Let’s be real: the FDA’s ‘80-125% bioequivalence’ range is a joke. That’s a 45% swing! Imagine if your insulin dose varied that much. Or your chemo. They call it ‘equivalent’-but it’s barely within the realm of medical sanity. This isn’t science. It’s corporate math.
And don’t even get me started on the ‘authorized generic’ loophole-same pill, same factory, same everything… just no logo. That’s not transparency. That’s a PR stunt.
And why do they still use lactose? So many people are intolerant. Nobody talks about that. Because it’s cheaper. And we’re all just supposed to swallow it. Pun intended.
They’re not educating us. They’re conditioning us to accept mediocrity.
Daz Leonheart-15 February 2026
Good read. I’ve been using generics for years and never had a problem. If you’re worried, ask your doc. But don’t let a different color scare you. Your health matters more than the brand on the bottle.