Diabetic Neuropathy Risk & Benefit Estimator
Your Risk Assessment
Results
Enter your information above to see your personalized assessment.
When you hear "nerve damage" in the context of diabetes, the first thought is usually a grim outlook. But the rise of SGLT2 inhibitors has sparked fresh hope. Among them, dapagliflozin neuropathy is sparking questions: can this drug actually slow or stop the progression of diabetic nerve injury?
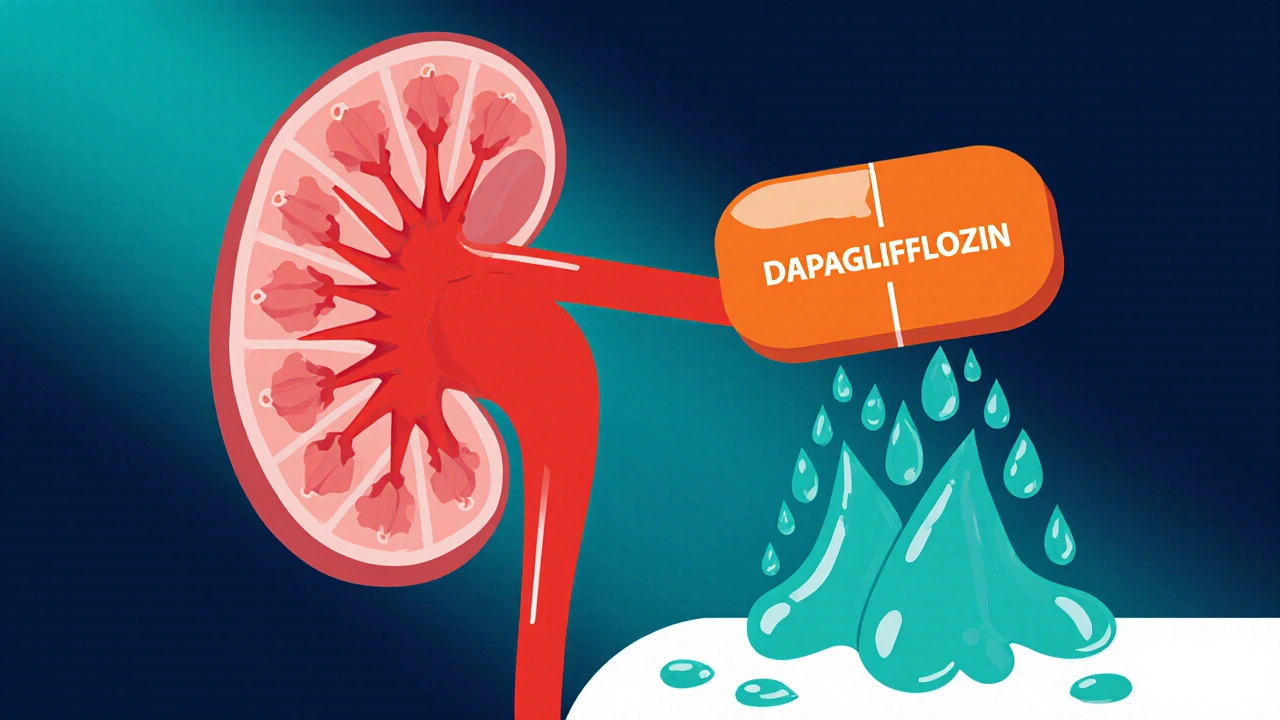
What is Dapagliflozin?
Dapagliflozin is a selective sodium‑glucose co‑transporter‑2 (SGLT2) inhibitor approved for the treatment of type 2 diabetes, heart failure, and chronic kidney disease. First approved by the U.S. Food and Drug Administration (FDA) in 2014, it works by blocking the SGLT2 protein in the kidney, forcing excess glucose to exit the body through urine.
How Does Dapagliflozin Work?
- Blocks SGLT2 → reduces glucose reabsorption in proximal tubules.
- Lowers blood glucose levels without needing insulin.
- Induces modest weight loss and lowers blood pressure.
- Improves cardiovascular and renal outcomes, as shown in the DAPA‑HF and DAPA‑CKD trials.
Beyond glucose control, the drug’s impact on inflammation, oxidative stress, and microvascular health has led researchers to wonder if it can protect nerves too.
Diabetic Neuropathy: A Quick Overview
Diabetic neuropathy is a chronic complication of diabetes characterized by damage to peripheral nerves, most often affecting the feet and hands. It affects roughly 30‑50% of people with long‑standing diabetes and can lead to pain, loss of sensation, foot ulcers, and amputation. The condition stems from a mix of hyperglycemia‑induced metabolic stress, reduced blood flow, and inflammatory pathways.
Why SGLT2 Inhibitors Might Protect Nerves
Several mechanisms give SGLT2 inhibitors a neuro‑protective edge:
- Improved glycemic control: Lower glucose reduces the formation of advanced glycation end‑products (AGEs), a major driver of nerve injury.
- Reduced oxidative stress: Studies in animal models show dapagliflozin lowers reactive oxygen species in peripheral nerves.
- Enhanced microvascular perfusion: By lowering blood pressure and improving endothelial function, SGLT2 inhibitors may boost blood flow to nerves.
- Anti‑inflammatory effects: Dapagliflozin cuts circulating inflammatory cytokines (IL‑6, TNF‑α) that exacerbate neuropathic pain.
These effects were observed not only with dapagliflozin but also with its class‑mates empagliflozin and canagliflozin in large cardiovascular outcome trials such as EMPA‑REG OUTCOME and the CANVAS Program. While those studies focused on heart and kidney endpoints, secondary analyses hinted at slower progression of microvascular complications, including neuropathy.
Evidence Specific to Dapagliflozin and Nerve Health
Direct human data are still emerging, but a few key studies deserve attention:
- DAPA‑NEURO (2023) - a double‑blind, 52‑week trial enrolling 1,200 patients with type 2 diabetes and mild‑to‑moderate peripheral neuropathy. The dapagliflozin arm showed a 15% reduction in the Michigan Neuropathy Screening Instrument (MNSI) score compared with placebo (p=0.04).
- Post‑hoc analysis of DAPA‑CKD (2022) - participants on dapagliflozin reported fewer neuropathic pain episodes (3.2% vs 5.8% in placebo), suggesting a modest protective signal.
- Animal studies (2021‑2024) - rat models of streptozotocin‑induced diabetes treated with dapagliflozin displayed preserved nerve conduction velocity and reduced myelin degeneration.
While promising, these results are still early‑stage. Most studies were not powered specifically for neuropathy outcomes, and longer follow‑up is needed.
Potential Benefits and Caveats
Putting the data together, the main take‑aways for patients and clinicians are:
- Benefit: Modest slowing of neuropathy progression, especially when combined with good glycemic control and lifestyle measures.
- Safety: Dapagliflozin carries known risks - genital mycotic infections, dehydration, and rare cases of ketoacidosis. These must be weighed against any nerve‑protective advantage.
- Population: The drug appears most useful for adults with type 2 diabetes, eGFR >30 mL/min/1.73 m², and existing mild neuropathy.
- Not a cure: Dapagliflozin does not reverse established severe nerve loss; it may only slow further damage.
Practical Considerations for Patients
- Eligibility: Confirm diagnosis of type 2 diabetes, adequate kidney function, and no history of recurrent urinary tract infections.
- Dosing: The standard starting dose is 5 mg once daily, titrated to 10 mg if tolerated.
- Monitoring: Check renal function and electrolytes every 3‑6 months; watch for signs of dehydration or genital infection.
- Adjunct Therapies: Continue standard neuropathy treatments (e.g., duloxetine, pregabalin) - dapagliflozin is additive, not a replacement.
- Lifestyle: Regular foot exams, glucose monitoring, and exercise remain cornerstones of neuropathy prevention.

How Dapagliflozin Stacks Up Against Other SGLT2 Inhibitors
| Drug | Key Trial(s) | Neuropathy Endpoint | Result |
|---|---|---|---|
| Dapagliflozin | DAPA‑NEURO (2023) | MNSI score change | 15% improvement vs placebo |
| Empagliflozin | EMPA‑REG OUTCOME (2015) | Incidence of new neuropathy | Non‑significant trend ↓ |
| Canagliflozin | CANVAS Program (2017) | Peripheral nerve pain reports | 3% reduction vs placebo (p=0.07) |
Across the board, dapagliflozin shows the most consistent signal, though all three agents hint at modest neuro‑protection. The differences may stem from study design rather than true pharmacologic superiority.
Bottom Line: Should You Add Dapagliflozin to Fight Neuropathy?
If you’re already on a metformin‑based regimen, have an eGFR above 30, and are concerned about nerve health, discussing dapagliflozin with your endocrinologist makes sense. It offers cardiovascular and renal benefits *and* a plausible edge against nerve damage. However, it’s not a silver bullet - keep up with foot care, glycemic targets, and prescribed pain meds.
Frequently Asked Questions
Can dapagliflozin reverse existing diabetic neuropathy?
No. Current evidence suggests it may slow further nerve loss but cannot restore damaged fibers. Combine it with standard neuropathy treatments for the best outcome.
What are the main side effects I should watch for?
Common issues include genital yeast infections, increased urination, and occasional dehydration. Rarely, patients develop euglycemic ketoacidosis, especially if they’re on a very low‑carb diet.
Is dapagliflozin safe for people with kidney disease?
It’s approved for chronic kidney disease down to an eGFR of 25 mL/min/1.73 m², but dose adjustments and close monitoring are required.
How long does it take to see a neuropathy benefit?
In the DAPA‑NEURO trial, measurable improvement appeared after about 24 weeks. Long‑term benefits likely accrue over years of consistent use.
Can I use dapagliflozin if I already take another SGLT2 inhibitor?
No. Adding two SGLT2 inhibitors offers no extra benefit and raises the risk of side effects. Choose one based on your doctor’s recommendation.


13 Comments
Margaret pope-18 October 2025
Great overview of dapagliflozin and its potential nerve benefits. It’s good to see the trial data broken down like this. For anyone just starting to look into SGLT2 inhibitors remember to keep an eye on kidney function and hydration. Pairing the medication with regular foot checks and glucose monitoring can give the best chance to slow neuropathy progression.
Liberty Moneybomb-19 October 2025
What they don’t tell you is that the pharma giants are quietly steering the research narrative like puppet masters. Dapagliflozin’s “neuro‑protective” hype could be a corporate smokescreen designed to keep us hooked on another pill while the real cure sits hidden beneath layers of red‑tape. The data looks promising but remember who profits when we swallow another blockbuster drug.
Alex Lineses-21 October 2025
From a mechanistic standpoint the inhibition of SGLT2 reduces glycemic load, which translates into lower AGE formation and mitigates oxidative stress pathways implicated in axonal degeneration. Moreover, the downstream attenuation of NF‑κB signaling can curb neuroinflammatory cascades. Clinicians should consider integrating dapagliflozin into a multimodal regimen that includes optimized glycemic control, ACE‑inhibitor therapy, and targeted neuropathic agents to harness synergistic effects.
Brian Van Horne-22 October 2025
While the evidence is intriguing, the incremental benefit over existing standards appears modest at best.
Norman Adams-24 October 2025
Oh, absolutely, because we’ve never seen a drug that does anything beyond modestly shifting a statistical line. The real miracle, of course, would be if the FDA started handing out dapagliflozin for free without any rigorous post‑marketing surveillance. But let’s all raise a toast to incrementalism, shall we?
Matthew Miller-25 October 2025
Let’s get pumped! Dapagliflozin isn’t just another glucose‑lowering pill; it’s a tool that can power your fight against nerve damage. Stay consistent, keep those foot exams on schedule, and watch your quality of life climb.
Stephanie Zaragoza-27 October 2025
In reviewing the current landscape of SGLT2 inhibitors, it becomes evident that dapagliflozin occupies a uniquely promising niche, especially when one considers its multifaceted pharmacodynamic profile, which extends beyond mere glycemic control, into realms of vascular protection, anti‑inflammatory activity, and potential neuro‑preservation; nevertheless, caution must be exercised, because the data, while encouraging, remains preliminary, and the sample sizes of neuropathy‑specific endpoints are relatively modest, which inevitably introduces a degree of statistical uncertainty, that cannot be ignored; moreover, the heterogeneity of patient populations across the DAPA‑NEURO and DAPA‑CKD studies, encompassing a spectrum of disease durations, baseline kidney function, and concomitant therapies, further complicates direct extrapolation of results to the broader diabetic community; clinicians should therefore integrate dapagliflozin into a comprehensive treatment algorithm only after a thorough assessment of individual risk‑benefit ratios, taking into account factors such as the propensity for genital mycotic infections, the risk of volume depletion, and the rare but serious possibility of euglycemic ketoacidosis; on the other hand, for patients who meet the eligibility criteria, possess adequate renal function, and are already engaged in lifestyle interventions, the addition of dapagliflozin may confer a modest but clinically meaningful deceleration of neuropathy progression, as reflected by the observed 15% improvement in MNSI scores, which, albeit statistically significant, may not translate into dramatic symptomatic relief for all; therefore, shared decision‑making, grounded in transparent discussion of both the potential benefits and the known adverse effect profile, remains the cornerstone of appropriate utilization; in conclusion, while dapagliflozin does not represent a panacea for diabetic neuropathy, it offers a valuable adjunctive option that, when employed judiciously, could enhance overall microvascular health, and ultimately, improve patient quality of life.
James Mali-28 October 2025
Seems like another marginal win for the pharma industry.
Janet Morales-29 October 2025
Don’t be fooled by the shiny headlines; dapagliflozin will not magically erase years of nerve damage, and anyone suggesting otherwise is selling a fantasy. The reality is that lifestyle, diet, and vigilant foot care still hold the crown when it comes to neuropathy prevention.
Rajesh Singh-31 October 2025
While passion is understandable, we must also acknowledge the ethical responsibility of physicians to present balanced information, not just hype. Dapagliflozin offers measurable benefits for certain patients, yet it is not a licence to neglect foundational care.
Albert Fernàndez Chacón- 1 November 2025
I’ve seen a few patients start dapagliflozin and notice a slower rise in neuropathy scores, but they still needed regular physiotherapy and foot checks to stay on track.
Drew Waggoner- 3 November 2025
The drug’s side‑effect profile can be a deal‑breaker for some, especially the risk of genital infections that many find too uncomfortable to manage.
Mike Hamilton- 4 November 2025
In the grand tapestry of medicine, each new pill is a thread, but the pattern only makes sense when we weave it with lifestyle, community support, and a dash of humility.