For decades, leukemia and lymphoma were treated with the same blunt tool: chemotherapy. It killed fast-growing cells-cancerous and healthy alike. Patients lost hair, fought nausea, and spent weeks in hospitals just to survive. But since 2001, when imatinib became the first targeted drug approved for chronic myeloid leukemia, everything changed. Today, we don’t just attack cancer-we outsmart it. Targeted therapies and cellular therapies are now reshaping survival, turning once-fatal diagnoses into manageable conditions-or even cures.
What Are Targeted Therapies, Really?
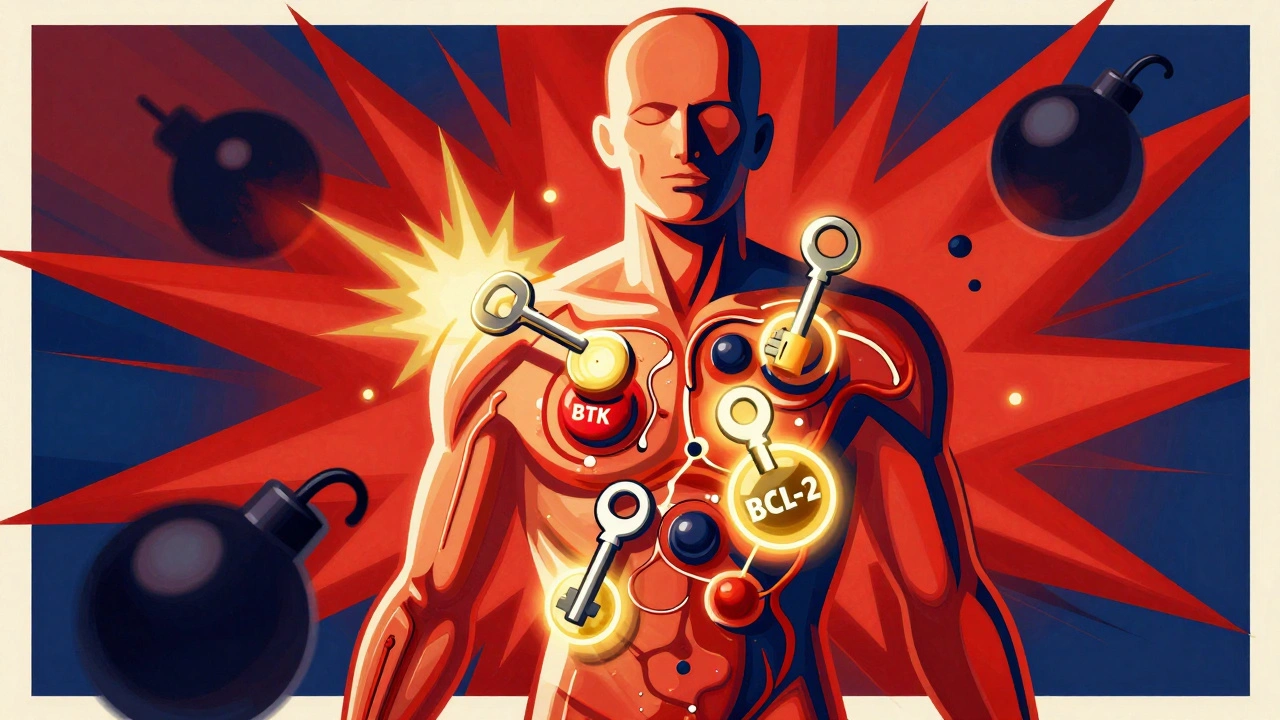
Targeted therapies are like precision keys that fit only one lock: the exact molecular flaw driving a cancer’s growth. Unlike chemo, which burns through the whole body, these drugs zero in on specific proteins or signals cancer cells depend on. For example, in chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL), two closely related diseases, the BTK protein acts like a fuel line for cancer cells. Drugs like ibrutinib and acalabrutinib block BTK, starving the cancer of its signal to multiply. Patients take them as pills-once a day, at home. No IVs. No hospital stays. Just a bottle and a routine. Another key player is venetoclax, which targets BCL-2, a protein that helps cancer cells avoid death. By flipping this survival switch, venetoclax forces malignant cells to self-destruct. Used with obinutuzumab or ibrutinib, it can deliver deep remissions in just 12 to 24 months. That’s a fixed-duration treatment-meaning patients stop after a set time, rather than taking pills for life. For many, this means no more daily medication, fewer side effects, and a real shot at long-term control.Cellular Therapy: Rewiring Your Immune System to Fight Cancer
If targeted therapies are precision tools, cellular therapies are biological superweapons. CAR T-cell therapy takes your own immune cells-T cells-and turns them into living drugs. Here’s how it works: First, your blood is drawn. T cells are separated out. In a lab, scientists add a synthetic receptor-called a chimeric antigen receptor, or CAR-that lets these T cells recognize CD19, a protein found on the surface of most B-cell lymphomas and leukemias. The cells are multiplied, then infused back into you. Once inside, they hunt down cancer cells like guided missiles. The first CAR T therapy, tisagenlecleucel (Kymriah), was approved in 2017 for kids with acute lymphoblastic leukemia. Today, we have three FDA-approved options: Kymriah, Yescarta (axicabtagene ciloleucel), and Breyanzi (lisocabtagene maraleucel). Each targets CD19, but they use slightly different engineering. Yescarta, for example, showed a 42.6% four-year survival rate in patients with relapsed large B-cell lymphoma after failing other treatments-something nearly unheard of just five years ago. Newer versions are even more advanced. Gilead’s KITE-363 and KITE-753 are dual-target CAR T therapies. Instead of just attacking CD19, they also target CD20. This reduces the chance of cancer escaping treatment by losing one antigen. Early results show 63.6% complete remission rates in patients who had exhausted all other options. One patient, a 58-year-old with mantle cell lymphoma that had spread after four prior therapies, achieved a complete response after a single infusion of LV20.19 CAR T cells-no signs of disease 18 months later.Why These Therapies Beat Old-School Chemo
Traditional chemoimmunotherapy for CLL and lymphoma often extended survival by a year or two-but at a high cost. Patients faced bone marrow suppression, infections, fatigue, and long hospital stays. The CLL Society’s 2025 data shows a dramatic shift: in the targeted therapy era, the median time from CLL diagnosis to Richter transformation (a deadly leap into aggressive lymphoma) jumped from 2.2 years to 4.9 years. That’s over two extra years of living with a manageable disease, not a ticking time bomb. For relapsed or refractory cases, CAR T-cell therapy crushes older salvage chemo regimens. In the ZUMA-7 trial, Yescarta doubled the rate of progression-free survival compared to standard chemo in second-line large B-cell lymphoma. And it’s not just about length-it’s about quality. Patients on targeted therapies often report near-normal energy levels. Many return to work, travel, or even coach their kids’ soccer teams. But it’s not all perfect. Targeted therapies can stop working. Resistance builds. Patients with del(17p) or TP53 mutations tend to progress faster on BTK inhibitors. That’s why doctors now combine therapies-like venetoclax plus ibrutinib-to delay resistance. And for those who do relapse, CAR T-cell therapy often remains an option.
The Real Cost: Money, Access, and Toxicity
These breakthroughs come with heavy price tags. A single CAR T-cell treatment costs between $373,000 and $475,000. Even with insurance, out-of-pocket costs can hit $15,000 to $25,000 per month for oral targeted drugs. That’s financial toxicity-a silent crisis. Many elderly patients with comorbidities face tough choices: take the drug and risk bankruptcy, or skip it and face the disease. And the side effects? They’re serious. CAR T-cell therapy can trigger cytokine release syndrome (CRS)-a storm of immune chemicals that causes high fever, low blood pressure, and organ stress. Neurotoxicity, including confusion, seizures, or trouble speaking, affects 20-40% of patients. These aren’t side effects you manage at home. They require ICU-level care. That’s why CAR T-cell therapy is only offered at certified centers. In the U.S., 89% of NCI-designated cancer centers offer it. But in rural areas or community clinics? Only 32% do. Targeted drugs aren’t risk-free either. Venetoclax can cause tumor lysis syndrome-when dying cancer cells flood the bloodstream with toxins. That’s why the first few doses are given in the hospital. Ibrutinib can cause bleeding, atrial fibrillation, and high blood pressure. Patients need regular monitoring: blood tests, EKGs, and check-ins with their oncologist.Who Gets These Therapies-and When?
Not everyone needs them. For newly diagnosed, low-risk CLL, watchful waiting is still standard. But for high-risk patients-those with del(17p), TP53 mutations, or rapid disease progression-targeted therapies are now first-line. CAR T-cell therapy is reserved for those who’ve failed at least two prior treatments. But that’s changing fast. In 2025, the FDA granted priority review to liso-cel (Breyanzi) for marginal zone lymphoma, with a decision expected by December. Meanwhile, clinical trials are testing CAR T-cell therapy in first-line treatment for aggressive lymphomas. A 2025 ASCO survey found 68% of hematologists believe CAR T-cell therapy will become standard first-line treatment for high-risk patients by 2030. Doctors are also exploring these therapies in rare forms like primary CNS lymphoma. Early results show promise. Some patients who had no options left-no chemo, no stem cell transplant-have responded to CAR T therapy injected directly into the spinal fluid.
The Future: Smarter, Safer, Earlier
The next wave of therapies is already here. Researchers are developing off-the-shelf CAR T cells-made from donor cells, not your own. That could cut manufacturing time from 3-5 weeks to days. There are also “armored” CAR T cells with added immune boosters, and CAR NK cells (natural killer cells) that may be safer and easier to store. Manufacturers are also trying to reduce toxicity. Newer CAR designs include safety switches-genes that can be turned off with a simple pill if side effects get too severe. Some trials are testing lower doses or split infusions to prevent CRS. One study showed that giving CAR T cells in two smaller doses, instead of one big one, cut severe side effects by half. And the data keeps improving. Real-world outcomes now match clinical trial results. A 2025 report from the Gene, Cell, & RNA Therapy Landscape showed 33 new non-genetically modified cell therapy trials launched in Q2 alone-most targeting solid tumors. That means the tools built for blood cancers are now being adapted for breast, lung, and pancreatic cancers.What This Means for Patients
If you or someone you love has leukemia or lymphoma, here’s the reality: You have more options than ever. But you also need to be proactive. Ask your oncologist: “Is my cancer being tested for genetic mutations? Am I a candidate for targeted therapy? Should I consider CAR T-cell therapy if this treatment fails?” Don’t wait until you’ve run out of options. For many, the best time to consider advanced therapy is at diagnosis-not after relapse. If your center doesn’t offer CAR T-cell therapy, ask for a referral. Many manufacturers have patient navigators who help with insurance, travel, and logistics. And remember: These aren’t magic bullets. But they’re the closest thing we’ve ever had to turning a death sentence into a life with meaning.What is the difference between targeted therapy and CAR T-cell therapy?
Targeted therapies are oral drugs that block specific proteins cancer cells need to grow, like BTK or BCL-2. They’re taken daily and work systemically. CAR T-cell therapy is a one-time infusion of your own modified immune cells that hunt and kill cancer. It’s more complex, requires hospitalization, and is used when other treatments fail. One is a pill; the other is a living drug.
Are targeted therapies better than chemotherapy?
For most patients with CLL, SLL, and certain lymphomas, yes. Targeted therapies often lead to longer remissions, fewer hospital visits, and less severe side effects than chemo. Studies show patients on BTK inhibitors or venetoclax live longer and report better quality of life. But they’re not always curative, and resistance can develop. Chemo still has a role in aggressive, fast-growing cases or when targeted drugs aren’t available.
Can CAR T-cell therapy cure leukemia or lymphoma?
For some, yes. In patients with relapsed or refractory B-cell acute lymphoblastic leukemia, up to 40% remain in remission five years after CAR T-cell therapy. In aggressive lymphomas like mantle cell lymphoma, complete responses are common-even after multiple relapses. While we don’t yet call it a “cure” for most, many patients live disease-free for years, sometimes decades, with no further treatment needed.
Why is CAR T-cell therapy so expensive?
It’s because it’s personalized medicine. Each treatment is made from your own cells, requiring specialized labs, genetic engineering, strict quality control, and trained staff. The process takes 3-5 weeks and involves multiple steps: leukapheresis, shipping, modification, expansion, and reinfusion. Plus, managing side effects requires ICU-level care. The cost reflects the complexity-not just the drug itself.
What if targeted therapy stops working?
If you develop resistance, your doctor will test for new mutations-like BTK or BCL-2 mutations-and switch you to another targeted drug or consider CAR T-cell therapy. Some patients respond to venetoclax after failing a BTK inhibitor, and vice versa. For those who’ve tried both, clinical trials for next-gen therapies or dual-target CAR T cells may be the best option.
Where can I get CAR T-cell therapy?
CAR T-cell therapy is only available at certified centers-usually large academic hospitals or NCI-designated cancer centers. These sites have the staff, ICU access, and experience to manage side effects. If your local oncologist doesn’t offer it, ask for a referral. Manufacturers like Kite and Novartis also provide patient support programs to help with travel, insurance, and logistics.
These therapies didn’t just extend life-they redefined it. What used to be a terminal diagnosis is now a journey with new milestones: a year without treatment, a child’s graduation, a trip overseas. The science is still evolving, but the message is clear: there’s hope, and it’s no longer a distant dream.




9 Comments
parth pandya- 2 December 2025
man i just read this whole thing and wow. i live in india and my uncle had CLL last year. they gave him ibrutinib and he’s been fine for 18 months now. no chemo no hair loss just a little diarrhea and he still plays cricket on weekends. this stuff is real. also typo: its BTK not BTK protein lol
Albert Essel- 2 December 2025
This is one of the most clearly written, clinically accurate summaries of modern hematologic oncology I’ve encountered on Reddit. The distinction between targeted therapies and CAR T-cell mechanisms is particularly well articulated. I especially appreciate the acknowledgment of financial toxicity and access disparities-these are the real ethical frontiers now.
Charles Moore- 2 December 2025
For anyone reading this and thinking ‘this sounds too good to be true’-it’s not. My sister was diagnosed with relapsed follicular lymphoma in 2021. After two lines of chemo failed, she got Yescarta. She had CRS, spent a week in ICU, but now? No cancer. No meds. Just regular checkups. She’s back to teaching kindergarten. This isn’t sci-fi-it’s Sunday dinner now.
Gavin Boyne- 3 December 2025
So we spent $500 billion on wars and got nothing but broken bodies, but somehow we can engineer a living missile from someone’s T cells to kill cancer? Yeah. Capitalism is wild. The real miracle isn’t the science-it’s that we’re only talking about this now after the billionaires got their own diagnoses.
Rashi Taliyan- 4 December 2025
I cried reading this. My cousin was 27 when she got diagnosed. They told her she had 18 months. Now? She’s 31. She got married last year. Her husband says she still screams when she sees a spider but she’s alive. I don’t care how much it costs-this is magic. Please don’t let money decide who lives.
Kara Bysterbusch- 4 December 2025
The transformation in clinical outcomes is nothing short of revolutionary. The transition from cytotoxic, non-selective interventions to precision molecular modulation and autologous cellular reprogramming represents a paradigmatic shift in therapeutic oncology. The emergence of dual-targeted CAR constructs and off-the-shelf allogeneic variants portends a future in which these modalities may be deployed with unprecedented scalability and safety.
Francine Phillips- 6 December 2025
so like... the pills work but they're expensive and the other thing is super expensive and you might die from it but it works? cool. i guess.
Katherine Gianelli- 7 December 2025
Reading this made me think of my grandma. She never got any of this. She had chemo in 2008, lost her appetite, slept 20 hours a day, and passed within a year. I wish she’d had even one of these options. I’m so glad people now get to live longer, fuller lives-but I can’t help feeling sad for everyone who came before. This progress matters. Don’t let it be just for the lucky ones.
Joykrishna Banerjee- 8 December 2025
LOL you all think this is groundbreaking? BTK inhibitors were discovered in 2004, CAR-T in 1989. The real innovation? Marketing. Pharma spent $12B on ads last year telling you ‘you deserve this’ while they jack up prices 700%. Also, del(17p) is still a death sentence if you’re uninsured. #CancerIsACapitalistTrap 😂