Medication Cognitive Risk Calculator
Medication Risk Assessment Tool
This tool helps you assess the cognitive risk of your medications. Many common drugs can cause brain fog and memory problems, especially anticholinergic drugs and certain other medications.
Your Cognitive Risk Assessment
What This Means
Recommendations
Many people notice something off after starting a new medication: they can’t remember where they put their keys, feel sluggish in the middle of the day, or struggle to follow a conversation. It’s not just aging. It’s not just stress. It could be the pills they’re taking. Brain fog and memory problems from medications are more common than most realize - and they’re often completely reversible.
What Does Medication-Induced Brain Fog Actually Feel Like?
It’s not the same as forgetting someone’s name. Medication-related brain fog feels like your thoughts are wrapped in cotton. You know the answer, but it’s just out of reach. You read the same sentence five times and still don’t absorb it. You walk into a room and forget why you’re there. These aren’t occasional slips - they’re persistent, frustrating, and interfere with daily life.
People describe it as mental slowdown. Like your brain is running on 50% battery. Some report sudden memory gaps - not just forgetting a name, but forgetting entire conversations or even driving routes. One Reddit user, after taking 5mg of Ambien for two weeks, described waking up with no memory of the night before. That’s not a dream. That’s anterograde amnesia - a known side effect of certain sleep meds.
Which Medications Are Most Likely to Cause These Problems?
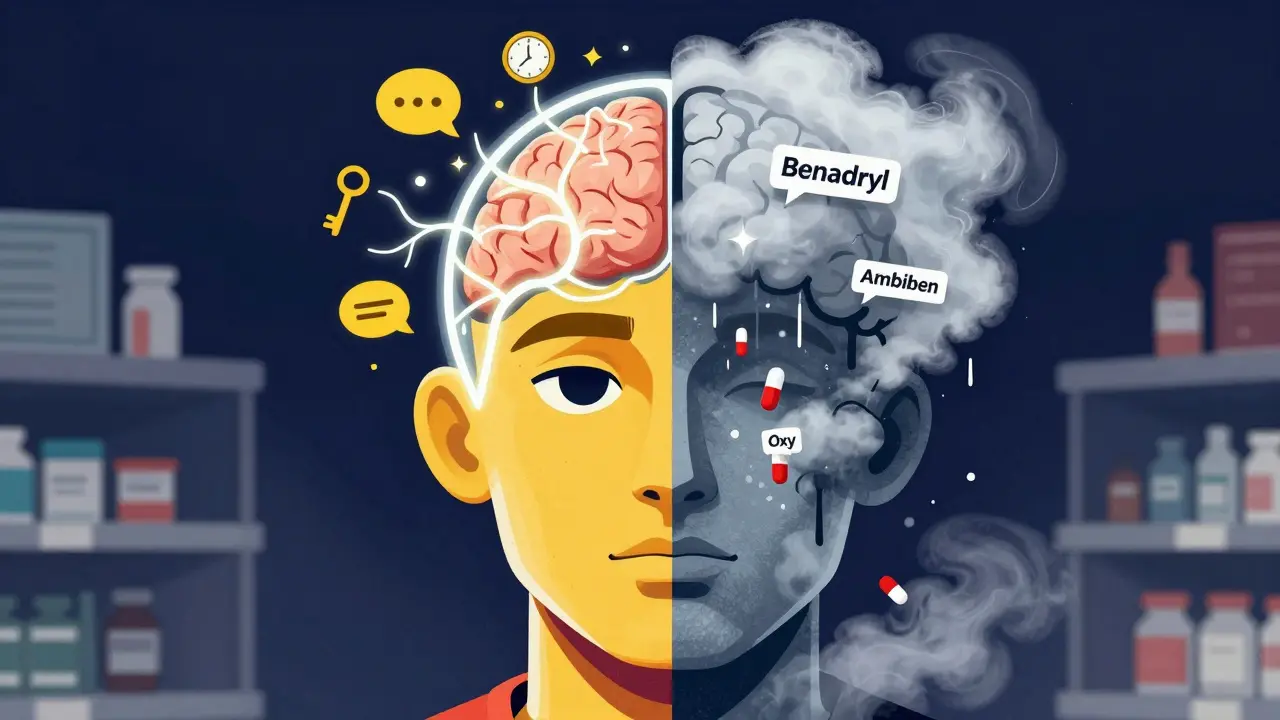
Not all drugs affect the brain the same way. Some are notorious for clouding cognition. The biggest culprits fall into a few clear categories:
- Anticholinergic drugs: These block acetylcholine, a key brain chemical for memory and focus. Common examples include diphenhydramine (Benadryl, Tylenol PM), oxybutynin (Ditropan for overactive bladder), and tricyclic antidepressants like amitriptyline. Studies show these can increase the risk of memory disorders by up to 4.5 times. Regular use of diphenhydramine over seven years raises dementia risk by 54%.
- Benzodiazepines and sleep hypnotics: Drugs like Xanax, lorazepam, and especially zolpidem (Ambien) reduce activity in the hippocampus - the brain’s memory center. Ambien users report memory blackouts in 15% of cases, compared to just 5% with older benzodiazepines.
- Opioid painkillers: Oxycodone, hydrocodone, and morphine disrupt working memory. Even at normal doses, they can cut memory capacity by 25%. Immediate-release versions hit harder than extended-release ones.
- Chemotherapy drugs: Known as “chemo brain,” this affects up to 75% of cancer patients. It’s not just fatigue - it’s trouble focusing, slower thinking, and memory lapses that can last months or years after treatment ends.
- Corticosteroids: Prednisone at doses above 20mg/day can trigger confusion, mood swings, and memory issues within days. These symptoms often mimic depression or dementia.
Here’s what’s surprising: some medications you wouldn’t expect are also on the list. Isotretinoin (for acne) and ciclosporin (for autoimmune conditions) have been linked to cognitive side effects. Even newer antidepressants like SSRIs can contribute, though less than older ones.
Why Do These Drugs Hurt Your Memory?
Your brain runs on chemicals - neurotransmitters - that send signals between cells. Medications interfere with this system in different ways.
Anticholinergics block acetylcholine. Without it, your brain struggles to form new memories. Benzodiazepines calm brain activity too much, especially in the prefrontal cortex and hippocampus - areas needed for focus and memory storage. Opioids bind to receptors in the medial temporal lobe, messing with how memories are consolidated. Chemo drugs damage neural networks directly. Even statins, often blamed for memory loss, show no real cognitive impact in large studies - so don’t panic if you’re on one.
The key point: these effects are usually reversible. Unlike Alzheimer’s, which slowly destroys brain tissue, medication-induced brain fog lifts when you stop or switch the drug.

Who’s Most at Risk?
Older adults are hit hardest. About 30% of seniors on multiple medications experience cognitive side effects. Why? Their bodies process drugs slower. Their brains are more sensitive. And they’re more likely to be taking several of these high-risk drugs at once - a dangerous combo.
But it’s not just seniors. Anyone on long-term pain meds, sleep aids, or antidepressants can be affected. A 68-year-old woman in a Pharmacy Times case study developed severe confusion after starting oxybutynin. Symptoms vanished within 10 days of stopping it. That’s not rare. AARP’s 2023 survey found 62% of adults over 50 blamed their memory problems on medications. Sleep aids, antihistamines, and painkillers were the top three.
How to Know If It’s Your Medication - Not Aging
Timing matters. If your brain fog started within days or weeks of beginning a new drug, that’s a red flag. If you feel clearer after skipping a dose (under medical supervision), that’s another clue.
Ask yourself:
- Did this start after a new prescription or OTC sleep aid?
- Do you feel better on weekends when you skip your meds?
- Are you taking more than three medications?
- Do you feel foggy only in the morning - even if you took the drug at night?
Also, check your meds for anticholinergic burden. Many online tools and pharmacy apps now calculate this. If your total score is high, talk to your doctor. The Beers Criteria, updated every two years, lists 52 drugs to avoid in older adults because of cognitive risks. Hospitals now use this to flag dangerous prescriptions.
What Can You Do? Practical Steps for Relief
Don’t stop cold turkey. But do take action.
- Make a full list of every medication - including vitamins, supplements, and OTC sleep aids. Many people forget the Benadryl they take for allergies or the Tylenol PM they use for occasional sleep.
- Ask your doctor to review it. Say: “I’ve been feeling mentally foggy since starting [drug]. Could this be related?” Don’t be shy. This is a common concern.
- Target the biggest offenders first. If you’re on diphenhydramine, switch to loratadine (Claritin) or cetirizine (Zyrtec) - they have almost no anticholinergic effect. For sleep, try melatonin (0.5-5mg) or trazodone (25-50mg). Both are much gentler on cognition.
- For pain, consider non-opioid options like duloxetine (Cymbalta). Studies show it causes 40% less cognitive impairment than opioids at similar pain relief levels.
- Timing matters. Take drowsy meds at bedtime. A Johns Hopkins study found this simple change reduced daytime brain fog by 35% in 78% of patients.
- Give it time. Once you stop or switch a drug, improvement usually starts in 3-7 days. Full recovery can take up to two weeks. Some cases, like chemo brain, take months.
Doctors now use tools like the Drug Burden Index and Anticholinergic Cognitive Burden (ACB) scale to measure risk. These are built into electronic health records at 87% of U.S. hospitals. If your doctor doesn’t mention them, bring it up.
New Hope: Better Drugs Are Coming
The medical world is waking up. In March 2024, the FDA required all benzodiazepines to carry warnings about memory loss. Pharmaceutical companies are rushing to develop safer alternatives. Seven new non-anticholinergic sleep drugs are in late-stage trials. One, daridorexant, shows 92% less cognitive impact than Ambien.
Even more promising: genetic testing. Your body’s ability to break down drugs depends on genes like CYP2D6 and CYP2C19. A 2023 study found these variants explain 40% of why some people get brain fog from meds and others don’t. University of Michigan’s 2024 trial showed that using this testing to guide prescriptions cut cognitive side effects by 63%.
And now, Medicare Part D will reimburse pharmacists for cognitive risk assessments starting in 2024. That means you’ll soon have access to expert medication reviews - not just from your doctor, but from your pharmacist too.
Final Thought: You’re Not Crazy
If you’ve been blaming yourself for forgetfulness, stop. You’re not losing your mind. You might just be taking the wrong pill. Medication-induced brain fog is real, common, and treatable. The first step is awareness. The second is asking the right questions. The third? Working with your doctor to find a solution that protects your brain - not harms it.
Don’t wait for it to get worse. Review your meds. Talk to your doctor. And remember: clarity doesn’t have to come with a side effect.
Can over-the-counter sleep aids cause memory problems?
Yes. Many OTC sleep aids, like Benadryl and Tylenol PM, contain diphenhydramine - a strong anticholinergic drug. Studies show regular use increases dementia risk by 54% over seven years. Even short-term use can cause memory blackouts and daytime brain fog. Switching to melatonin or trazodone offers sleep support without the cognitive cost.
How long does it take for brain fog to go away after stopping a medication?
It varies. For most people, improvement starts within 3-7 days after stopping or reducing the drug. Full recovery usually takes 1-2 weeks. For drugs like benzodiazepines or opioids, withdrawal can cause temporary worsening before improvement. Chemo brain may take months to improve. If symptoms don’t lift after 4 weeks, other causes should be checked.
Are antidepressants linked to memory loss?
Older antidepressants like amitriptyline (a tricyclic) have strong anticholinergic effects and are strongly linked to memory problems. Newer ones like SSRIs (e.g., sertraline, fluoxetine) have much lower risk - about 1.8 times higher than non-users, compared to 4.2 times for tricyclics. If you’re on an older antidepressant and notice fog, ask about switching to an SSRI or SNRI like venlafaxine.
Can statins cause brain fog?
Some people report memory issues with statins, but large studies show no significant difference in cognitive function between statin users and placebo groups after six months. Case reports exist, but they’re rare - affecting only 1-2% of users. If you suspect your statin is the cause, talk to your doctor before stopping. The heart benefits usually outweigh the tiny risk of cognitive side effects.
What’s the best way to check if my meds are causing brain fog?
Start by listing every medication you take, including OTC and supplements. Use an anticholinergic burden calculator (available online or through your pharmacy). Ask your doctor to review your list using the Beers Criteria. Consider a medication review with your pharmacist - now covered by Medicare. Track your symptoms: do they improve on days you skip a pill? That’s a strong indicator.


12 Comments
Mussin Machhour-24 December 2025
Been there. Took Ambien for a week after my mom passed and woke up like I’d been hit by a bus. Couldn’t remember my own phone number for two days. Switched to melatonin - zero brain fog, still sleep like a baby. Why do doctors still push these toxic sleep aids? It’s insane.
Oluwatosin Ayodele-25 December 2025
Let’s be real - most of this is just Big Pharma covering their tracks. Anticholinergics? Of course they cause brain fog. They’ve known this since the 80s. But why? Because dementia = more prescriptions for more drugs. It’s a cycle. Your ‘reversible’ brain fog? It’s just the first stage. Once your acetylcholine’s fried, it doesn’t come back. They’ll sell you a $500 supplement next month to ‘fix’ what they broke.
Rick Kimberly-26 December 2025
While the general observations presented are empirically sound and align with current pharmacological literature, one must exercise caution in extrapolating causality from anecdotal reports. The Beers Criteria, while widely adopted, remains a consensus-based guideline rather than an evidence-based algorithm. Furthermore, the temporal association between medication initiation and cognitive decline does not inherently establish a causal relationship absent controlled longitudinal data.
Linda B.-27 December 2025
Did you know the FDA knew about Ambien’s memory blackouts since 2007 but didn’t warn the public until 2024? Why? Because the pharmaceutical lobby donated $200 million to politicians that year. They’re not protecting your brain - they’re protecting their stock price. Your ‘reversible’ brain fog? It’s just the tip of the iceberg. Next they’ll say your depression is caused by your meds too - because it is. And they’ll sell you another pill to fix it
Christopher King-29 December 2025
THIS IS THE NEW EUGENICS. They’re drugging the masses into compliance. Anticholinergics? Benzodiazepines? Chemo brain? It’s not medicine - it’s mind control. They want us docile. Forgetful. Quiet. Look at the numbers - 62% of seniors blame meds for memory loss? That’s not coincidence. That’s design. They’re not treating illness - they’re creating dependency. Wake up. The system is rigged. Your brain is a battlefield. And they’re winning.
Gary Hartung-30 December 2025
While I appreciate the article’s attempt at clarity, it remains fundamentally superficial. The underlying neuropharmacological mechanisms - particularly the role of GABA-A receptor modulation in benzodiazepine-induced hippocampal suppression - are reduced to bullet points. Furthermore, the omission of CYP450 polymorphism interactions renders the ‘genetic testing’ section dangerously reductive. One cannot reduce cognitive risk to a single score. The human brain is not a spreadsheet.
Ben Harris-31 December 2025
My ex-wife took 50mg of prednisone for her ‘allergies’ - she forgot our wedding anniversary, called me by her dog’s name, and tried to pay the cable bill with a credit card she’d shredded. She cried for three days after stopping it. But no one told her. No one warned her. The doctors just shrugged. That’s not medicine. That’s negligence. And now I’m scared to take anything. Even Advil. What if it’s the one that makes me forget my own name?
Jason Jasper-31 December 2025
I’ve been on a statin for 10 years. Thought I was getting forgetful. Took a 2-week break - nothing changed. Then I realized I was just tired from working two jobs and not sleeping. Sometimes it’s not the pill. It’s life. Don’t panic. Track it. Talk to someone. But don’t assume every foggy day is a drug reaction. Your brain’s tired - not broken.
Carlos Narvaez- 1 January 2026
Melatonin works. Trazodone works. Benadryl doesn’t. End of story.
Harbans Singh- 2 January 2026
As someone from India, I’ve seen this with my grandmother - she was on multiple antihistamines for allergies and started forgetting her own children’s names. We switched her to cetirizine, and within 10 days, she was back to telling stories from her childhood. It’s not just a Western problem. This is global. But here, no one talks about it. Doctors just say ‘it’s age.’ Please share this. More people need to know.
Justin James- 4 January 2026
They’re not just drugging you - they’re drugging your kids. Look at the school lunch programs - they’re laced with anticholinergics in processed foods. The same chemicals they put in Benadryl are in your kid’s cereal. They want a generation that can’t think critically. That’s why they’re pushing sleep meds, antidepressants, and painkillers - it’s all connected. The government knows. The doctors know. But they won’t tell you because they’re paid by the same companies that make the pills. The FDA? A joke. The Beers Criteria? A Band-Aid on a bullet wound. They’re turning America into a walking zombie zone. And you’re still taking your Tylenol PM like it’s harmless. Wake up. It’s not a sleep aid. It’s a cognitive suppressant.
Zabihullah Saleh- 4 January 2026
In my culture, we say: ‘The body remembers what the mind forgets.’ When I stopped my antidepressant, I didn’t just feel clearer - I felt like I was coming home. Like I’d been living in a foggy room for years and someone finally opened the window. It wasn’t the pill that made me sad - it was the pill that made me numb. And numbness isn’t peace. It’s silence. And silence is the loudest kind of pain.