Diarrhea hits hard and fast. One minute you’re fine, the next you’re racing to the bathroom. It’s common, usually harmless, and often gone in a day or two. But when it’s bad, you want relief-fast. That’s why millions reach for OTC diarrhea treatments like Imodium or Pepto-Bismol. They work. But they’re not magic pills. Using them wrong can make things worse. Knowing when to take them-and when to walk away from the pharmacy shelf-is the difference between quick relief and a trip to the ER.
What OTC Diarrhea Medicines Actually Do
There are two main types of OTC diarrhea treatments you’ll find on the shelf: loperamide and bismuth subsalicylate. They work in totally different ways, and that matters.
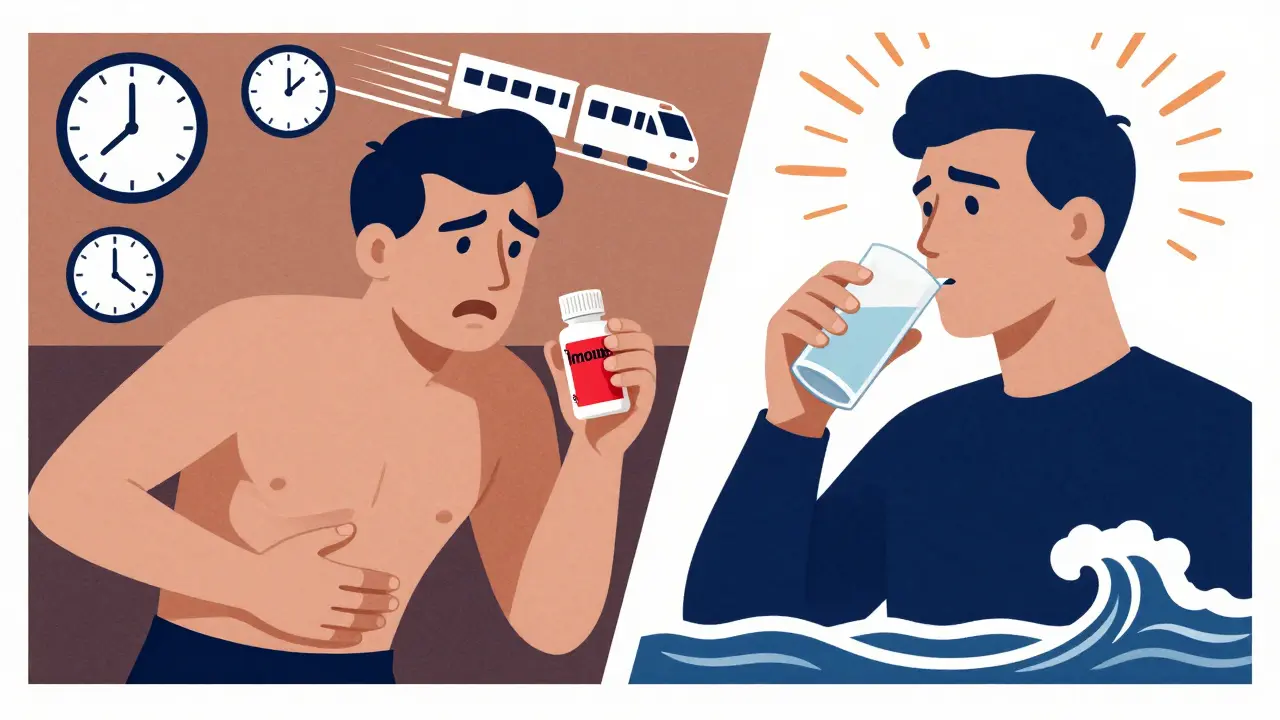
Loperamide, sold as Imodium, slows down your gut. It doesn’t cure the cause of diarrhea-it just makes your intestines move slower. That means fewer trips to the bathroom. Studies show it cuts stool frequency by about 60% within 24 hours. It kicks in within 30 to 60 minutes. That’s why people swear by it when they’re stuck on a long flight or at work.
Bismuth subsalicylate, the active ingredient in Pepto-Bismol and Kaopectate, does more than slow things down. It coats your gut, reduces inflammation, fights certain bacteria like E. coli, and even helps with nausea and cramps. About 48% of users see fewer bowel movements, but 37% also report less nausea. It’s the better choice if you’re feeling sick all over, not just having loose stools.
Both are available in pills, liquids, and chewables. Imodium caplets contain 2mg of loperamide. Pepto-Bismol chewables give you 262mg of bismuth subsalicylate per tablet. Always check the label. Dosing isn’t the same across brands.
When It’s Safe to Use OTC Treatments
If your diarrhea started suddenly, you don’t have a fever, and there’s no blood in your stool, you’re likely dealing with a mild viral bug or food intolerance. This is where OTC meds shine.
For loperamide: Take 4mg after your first loose stool. Then take 2mg after each new loose stool-but never more than 8mg in 24 hours. That’s the legal limit for OTC sales in the U.S. after the FDA cracked down on abuse in 2016. Too much can mess with your heart rhythm. There have been deaths linked to people taking 50, 100, even 200mg a day to self-treat opioid withdrawal. That’s not diarrhea treatment. That’s dangerous.
For bismuth subsalicylate: Take 30mL of liquid or two chewable tablets after each loose stool, up to eight doses in 24 hours. It’s fine for adults and teens 12+. Kids under 12 need a different formula. Don’t give adult Pepto-Bismol to a child-it contains salicylate, which can cause Reye’s syndrome, a rare but serious condition.
Side effects? Loperamide can cause constipation. One in eight users gets stuck. Bismuth subsalicylate turns your stool black and your tongue gray. It’s harmless, but it freaks people out. Don’t panic. It’s just bismuth. You’ll see it in the mirror and think you’re dying. You’re not.
When OTC Treatments Are a Bad Idea
Don’t take either of these if you have:
- A fever higher than 100.4°F (38°C)
- Bloody or black, tarry stools
- Severe abdominal pain or swelling
- Diarrhea lasting more than 48 hours
These aren’t just inconveniences. They’re red flags. Fever and blood mean your body is fighting something serious-like salmonella, shigella, or C. diff. Slowing your gut down with loperamide traps those bugs inside. That’s like locking the door while the thief is still inside. The Mayo Clinic, NHS, and American Gastroenterological Association all agree: don’t use anti-diarrheals if you have these symptoms.
There’s also a hidden risk with bismuth subsalicylate: if you’re already taking aspirin or other NSAIDs, you could be doubling up on salicylates. That raises your risk of stomach bleeding or kidney damage. Check all your meds. Even if it’s just a baby aspirin for heart health, talk to a pharmacist before mixing.
What You Should Be Doing Instead
Medicines help with symptoms. But your body needs hydration to heal. That’s the real key.
Drink oral rehydration solutions (ORS). These aren’t just water. They’re a precise mix of salts and sugars that your gut can absorb fast. WHO guidelines recommend 75mmol/L sodium. You can buy packets (like Pedialyte or Dioralyte) or make your own: 1 liter of clean water, 6 teaspoons of sugar, half a teaspoon of salt. Sip it slowly. Don’t chug. Chugging makes you vomit.
Stop dairy, caffeine, alcohol, and high-fiber foods for a day or two. They irritate your gut. Stick to the BRAT diet: bananas, rice, applesauce, toast. Simple, bland, easy to digest. Most pediatricians still recommend this. Even though some newer studies question it, 92% of them still do.
Rest. Your body is fighting an infection. Pushing through work or exercise won’t help. Sleep, hydrate, wait it out.
Who’s at Higher Risk?
Not everyone handles diarrhea the same way.
Children under 6: Their bodies lose fluids faster. A 10-pound baby losing 10% of their body weight in fluids is in danger. Don’t give them OTC meds without a doctor’s go-ahead.
Older adults: Kidneys don’t work as well. They’re more prone to dehydration and electrolyte imbalances. A single day of diarrhea can land them in the hospital.
People with chronic illnesses: Diabetes, kidney disease, heart failure-these make dehydration more dangerous. Even mild diarrhea can trigger complications.
Travelers: If you’re in a country with questionable water, bismuth subsalicylate can reduce your risk of traveler’s diarrhea by up to 65%. Take it before meals. But if you get sick anyway, don’t push through. Hydrate. Rest. See a doctor if it lasts more than 48 hours.
Why People Get It Wrong
Most people start with the right dose. But they don’t stop when they should.
Amazon reviews show 32% of Imodium users say they got constipated. That’s not a side effect-it’s a warning sign. You’re not supposed to feel like you’re blocked up. If you haven’t had a bowel movement in 48 hours after stopping diarrhea, you’ve gone too far.
Reddit threads are full of stories: “Took 6 Imodium caplets in 4 hours-ended up in ER.” “My dad took it for a week because he didn’t want to miss work.” “I used it to calm my anxiety.”
These aren’t just mistakes. They’re patterns. People treat diarrhea like a nuisance, not a signal. But your gut is trying to tell you something. Sometimes, it’s just bad sushi. Sometimes, it’s something bigger.
When to Call a Doctor
Here’s the simple checklist:
- Diarrhea lasts more than 2 days
- You’re dizzy, lightheaded, or can’t keep fluids down
- Your urine is dark or you haven’t peed in 8 hours
- You’ve lost more than 5% of your body weight (e.g., 7 pounds if you weigh 140)
- You have a fever over 101.3°F (38.5°C)
- There’s blood or pus in your stool
- You’re pregnant, elderly, or have a weakened immune system
If any of these apply, stop the OTC meds. Call your doctor. Go to urgent care. Don’t wait. Dehydration kills. Infections like C. diff or cholera can spread fast.
And if you’ve been taking loperamide for more than a week, even if you feel fine, talk to a doctor. Long-term use can cause intestinal paralysis or heart problems. It’s rare, but it happens.
The Bigger Picture
OTC diarrhea treatments are a $1.2 billion market in the U.S. alone. Four in ten adults use them before even thinking about seeing a doctor. That’s normal. But it’s also why we need better education.
Most people know how to take the first dose. Only 43% know when to stop. That’s a gap. And it’s dangerous.
Medicine isn’t just about pills. It’s about listening to your body. Diarrhea isn’t the enemy. Ignoring the warning signs is.
Use OTC meds wisely. Hydrate like your life depends on it-because it does. And if things don’t improve? See a doctor. No shame in it. Your gut will thank you.
Can I give Imodium to my child?
Only if it’s the specific pediatric formulation and your child is at least 6 years old. Never give adult Imodium caplets to a child under 12. Loperamide can cause paralytic ileus in young kids, a dangerous condition where the intestines stop moving. The FDA has received over 120 reports of serious reactions in children between 2010 and 2020. Always check the label and talk to a pediatrician first.
Is Pepto-Bismol better than Imodium for traveler’s diarrhea?
For prevention, yes. Taking bismuth subsalicylate before meals can reduce your risk of traveler’s diarrhea by up to 65%. For treatment, it’s a tie. Imodium reduces stool frequency more sharply, but Pepto-Bismol also helps with nausea and cramps. If you’re feeling sick all over, Pepto-Bismol gives you more relief. But if you just need to stop the runs fast, Imodium works quicker. Neither treats the infection-just the symptoms.
Why does my stool turn black after taking Pepto-Bismol?
It’s harmless. Bismuth subsalicylate reacts with sulfur in your digestive tract to form bismuth sulfide, a black compound. About 98% of users see black stools, and 85% get a grayish tongue. It’s not bleeding. It’s not cancer. It’s just chemistry. The color fades within a day or two after you stop taking it. But if your stool stays black after you’ve stopped Pepto-Bismol, see a doctor-true black, tarry stool can mean internal bleeding.
Can I take loperamide and Pepto-Bismol together?
No. Don’t combine them. Loperamide slows your gut. Pepto-Bismol contains salicylate, which can irritate your stomach lining. Taking both increases your risk of side effects like constipation, nausea, and stomach bleeding. There’s no proven benefit. If one isn’t working, wait. Hydrate. Rest. If symptoms persist, see a doctor instead of stacking meds.
What’s the safest way to rehydrate during diarrhea?
Use an oral rehydration solution (ORS) with the right balance of salt and sugar: 75mmol/L sodium, 75mmol/L glucose. You can buy ready-made packets like Pedialyte or Dioralyte, or make your own: mix 1 liter of clean water, 6 teaspoons of sugar, and half a teaspoon of salt. Sip slowly-about 1 cup every hour. Avoid sports drinks, soda, and juice. They have too much sugar and not enough electrolytes, which can make diarrhea worse.
How long should I wait before seeing a doctor if OTC meds don’t work?
If your diarrhea lasts more than 48 hours, or if you develop fever, blood in stool, dizziness, or can’t keep fluids down, see a doctor immediately. Waiting longer increases your risk of dehydration or complications like C. diff or bacterial infection. OTC meds are for short-term relief, not long-term fixes. If your body hasn’t bounced back in two days, it’s not just a bug-it’s something that needs medical attention.



11 Comments
Paul Barnes-19 January 2026
Let’s be clear: loperamide is not a cure. It’s a temporary bandage. And yet, people treat it like a magic bullet. The FDA limit of 8mg/day exists for a reason-overuse causes cardiac arrhythmias. I’ve seen ER reports. It’s not dramatic. It’s predictable. Stop treating your gut like a broken faucet you can just turn off.
Thomas Varner-19 January 2026
Honestly? I just chug Pedialyte and wait it out. No meds. No drama. My body knows what to do. I used to take Imodium every time I ate something weird... now I just sip electrolytes, nap, and let it run its course. Surprisingly, I feel better faster. Also: black stools? Yeah, I thought I was dying. Turns out, it’s just bismuth. Weird, but harmless. 😅
Andy Thompson-20 January 2026
EVERYONE KNOWS THE GOVERNMENT PUT A LIMIT ON IMODIUM BECAUSE THEY WANT YOU TO GO TO THE DOCTOR AND PAY $$$! 🤡 They don’t care if you’re stuck on a plane-they care about your insurance bill. And don’t get me started on Pepto-Bismol-bismuth? That’s a metal! They’re poisoning us with heavy metals under the guise of ‘relief’! 🚨
sagar sanadi-21 January 2026
Why do Americans always need a pill for everything? In India, we drink buttermilk with ginger and salt. Works better. Also, no one dies from diarrhea here. You just rest. Maybe your body is trying to tell you to eat less junk food? 🤔
kumar kc-23 January 2026
Using OTC meds without understanding the cause is reckless. Period.
thomas wall-24 January 2026
It is, quite frankly, a national disgrace that the average citizen treats gastrointestinal distress as a trivial inconvenience, rather than a physiological signal demanding respect. The casual misuse of loperamide, often in conjunction with caffeine and alcohol, reflects a broader cultural decay in personal responsibility and medical literacy. One does not simply ‘pop a pill’ and ignore the body’s alarm systems. The Mayo Clinic, the NHS, and the AGA are not exaggerating-these are not recommendations; they are ethical imperatives. To treat diarrhea as a nuisance is to treat one’s own physiology with contempt.
Edith Brederode-26 January 2026
I used to take Imodium before flights and then felt guilty for days 😅 But after reading this, I switched to ORS and now I actually feel like I’m helping my body heal-not just hiding the symptoms. Also, black poop? I thought I was dying. Then I laughed. Now I just say ‘bismuth vibes’ and move on. 🙌
clifford hoang-28 January 2026
Think about it-why do these pills work so fast? Because they’re suppressing your body’s natural detox mechanism. 🤯 The pharmaceutical industry doesn’t want you to heal-they want you to stay dependent. Loperamide? It’s a synthetic opioid analog. They’re literally giving you a mild opiate to stop your bowels. And you’re thanking them? 😏 Wake up. The ‘diarrhea crisis’ is manufactured. They profit from your fear. Your gut is trying to purge toxins-maybe from GMOs, maybe from fluoride, maybe from 5G. Don’t silence it. Listen to it. 🧠
Arlene Mathison-29 January 2026
Y’all are overthinking this. Drink water. Eat bananas. Don’t panic. Your body’s got this. I’ve had diarrhea for 3 days once-no meds, just rest and broth-and I felt better by day 4. You don’t need to be a scientist to know when to hydrate. Sometimes, the best medicine is just… chilling. 🌿
Art Gar-31 January 2026
While the pharmacological mechanisms of loperamide and bismuth subsalicylate are well-documented, the sociological implications of their widespread, unsupervised use warrant deeper scholarly inquiry. The normalization of self-diagnosis and self-medication, particularly within the context of consumerist healthcare paradigms, represents a significant epistemological shift in public health discourse. One must question whether the proliferation of OTC remedies has inadvertently eroded the public’s capacity for physiological self-awareness and clinical deference.
Emily Leigh- 1 February 2026
Okay, but… why does everyone act like diarrhea is some kind of moral failure? 😒 I had it after a burrito. Big deal. I took Pepto. I drank water. I didn’t die. I didn’t need a PhD to figure it out. People treat this like it’s a crisis… it’s just a gross Tuesday. Also, black poop? Yeah, I’ve seen it. It’s gross. But I Google it and it’s ‘bismuth.’ So… cool. I’m not a doctor. I’m just a person who ate bad tacos. Chill out.