Every year, tens of thousands of people end up in the emergency room-not because of an accident, but because they took two different pills that contained the same active ingredient. It’s not rare. It’s not complicated. And it’s almost always preventable.
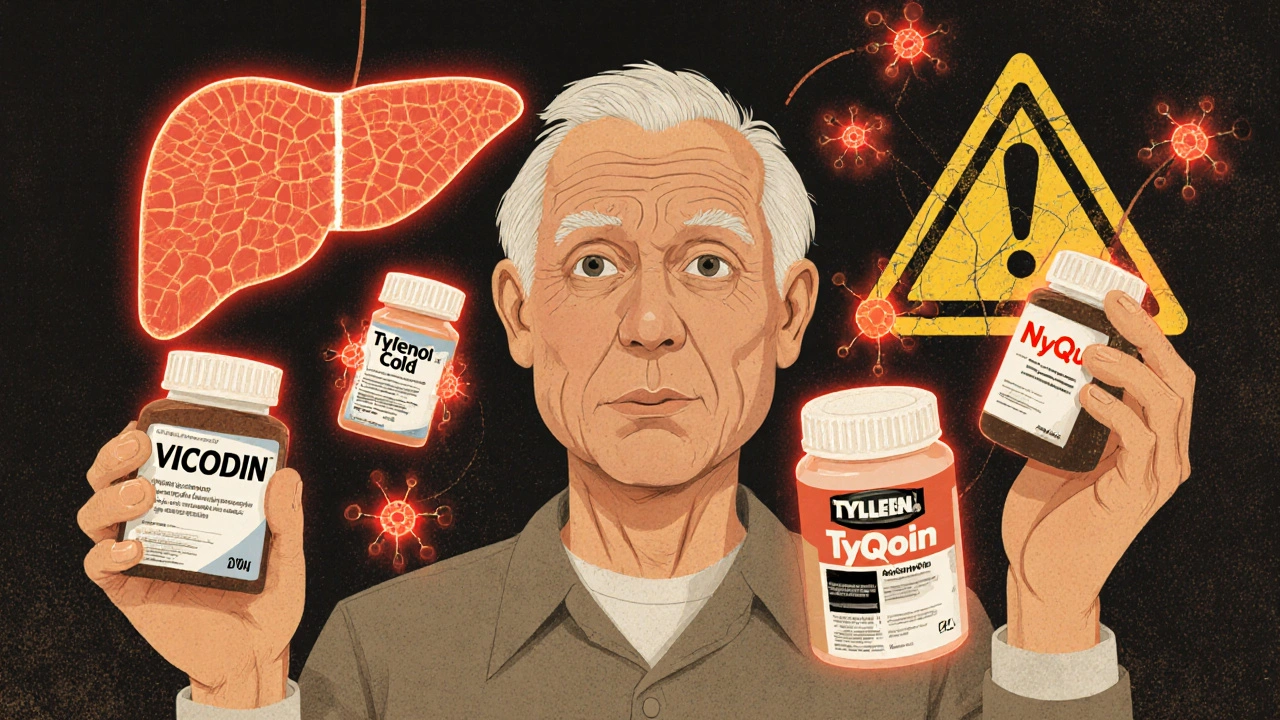
You might be taking a prescription painkiller like Vicodin for back pain. At the same time, you grab a bottle of Tylenol Cold from the shelf because you’ve got a stuffy nose. Both contain acetaminophen. You don’t think twice. But if you take both, you could easily hit the maximum safe daily dose-4,000 milligrams-without even realizing it. And that’s when your liver starts to fail.
This isn’t a hypothetical risk. In the U.S., acetaminophen causes more than 56,000 emergency visits every year from unintentional overdose. The majority of those cases happen because people don’t know they’re doubling up. And it’s not just acetaminophen. The same thing happens with diphenhydramine (found in sleep aids and allergy meds), pseudoephedrine (in cold and sinus remedies), and NSAIDs like ibuprofen or naproxen (in pain relievers and anti-inflammatories).
Why This Happens More Than You Think
Most people who take multiple medications aren’t careless. They’re just confused. There are too many brands, too many names, and too little clear labeling. A 2022 FDA review found that 45% of prescription labels don’t mention whether the drug shares ingredients with common over-the-counter products. Meanwhile, 68% of people don’t tell their doctors they’re using herbal supplements or OTC meds-because they don’t think it matters.
Older adults are hit hardest. About 40% of Americans over 65 take five or more medications regularly-a condition called polypharmacy. And 65% of hospitalizations from double ingredient errors happen in this group. Why? Because they often see multiple specialists. One doctor prescribes a blood pressure pill. Another prescribes a sleep aid. A third prescribes a painkiller. None of them know what the others have written. And if you’re filling prescriptions at different pharmacies, the system can’t catch the overlap.
One Reddit user, ‘MedSafety101,’ shared a story that got over 2,300 upvotes. He took three different cold medicines-all containing pseudoephedrine-because he thought each one was for a different symptom. He ended up with dangerously high blood pressure and had to be rushed to the ER. He wasn’t reckless. He just didn’t know.
The Most Dangerous Double Ingredients
Some ingredients are riskier than others. Here are the top three you need to watch for:
- Acetaminophen (also called paracetamol): Found in over 600 OTC and prescription products, including Tylenol, Percocet, Vicodin, Excedrin, and many cold and flu remedies. The safe daily limit is 3,000-4,000 mg. Exceeding that can cause irreversible liver damage.
- Diphenhydramine: An antihistamine that causes drowsiness. It’s in Benadryl, NyQuil, ZzzQuil, and many sleep aids. If you’re also taking a prescription sedative like benzodiazepines or sleep pills, the combined effect can slow your breathing to dangerous levels.
- NSAIDs (ibuprofen, naproxen, diclofenac): Found in Advil, Aleve, Motrin, and many arthritis or pain relief formulas. Taking two NSAIDs together-or one NSAID with aspirin-raises your risk of stomach bleeding, kidney damage, and heart problems.
The American Geriatrics Society’s Beers Criteria® lists 30 medication classes with high double ingredient risk. Twelve of those involve combinations of sedatives, antihistamines, and painkillers that are especially dangerous for older adults.

How to Protect Yourself
You don’t need to be a pharmacist to avoid this. Just follow these five steps:
- Make a full list of everything you take. Not just prescriptions. Include every OTC pill, vitamin, herb, supplement, and even eye drops or patches. Write down the name, dose, and how often you take it. Keep a copy in your wallet and another at home.
- Take your list to every doctor visit. Don’t wait for them to ask. Say: “Here’s everything I’m taking. Can you check for overlaps?” Studies show this reduces double ingredient errors by 78%.
- Use one pharmacy for all your medications. If you get prescriptions from multiple doctors, fill them all at the same pharmacy. Their system flags dangerous combinations automatically. A 2021 JAMA study found this cuts double ingredient risks by 63%.
- Ask your pharmacist: “Does this interact with anything else I’m taking?” Pharmacists catch 87% of double ingredient issues during medication reviews. They’re trained for this. Use them.
- Check OTC labels like a detective. Look for the “Active Ingredients” section. If you see the same name on two different bottles, don’t take both. Even if the brand names are different-like “Store Brand Cold & Flu” and “Tylenol Cold”-if they both list acetaminophen, you’re doubling up.
What’s Changing to Help
Things are getting better, but slowly. The FDA launched its Over-the-Counter Drug Facts Label Modernization Initiative in January 2024. By December 2025, all OTC products must display active ingredients in a clearer, standardized format. No more hiding them in tiny print.
Electronic health records from Epic and Cerner now include “double ingredient check” alerts. When a doctor prescribes a new drug, the system scans your list and warns if there’s a duplicate. But here’s the catch: those alerts only work if your OTC meds are in the system. And right now, only 43% of EHRs actually track them.
Apple Health, integrated into iOS 17, now flags duplicate ingredients when you enter your meds. You can scan a pill bottle or type in the name, and it will warn you if you’re taking two things with the same active ingredient. It’s not perfect-but it’s a start.

What to Do If You’ve Already Overdosed
If you think you’ve taken too much acetaminophen, don’t wait for symptoms. Go to the ER immediately. Liver damage from acetaminophen doesn’t show up right away. You might feel fine for 24 hours. Then nausea, vomiting, and jaundice hit. By then, it’s too late.
For sedatives: If you feel extremely drowsy, confused, or have trouble breathing after mixing meds, call emergency services. Don’t try to sleep it off. Respiratory depression can be fatal.
For NSAIDs: If you notice black, tarry stools, stomach pain, or dizziness after taking multiple painkillers, get checked. These are signs of internal bleeding.
Final Reality Check
You don’t need to stop taking your meds. You just need to know what’s in them. Double ingredient errors are the most preventable kind of medication harm. The National Coordinating Council on Medication Error Reporting and Prevention says 89% of these cases could be avoided with a simple, updated list.
It’s not about being perfect. It’s about being aware. One list. One pharmacy. One conversation with your pharmacist. That’s all it takes to avoid a hospital visit you never saw coming.
Can I take two different brands of the same OTC medicine if they’re for different symptoms?
No. Even if one is for a cold and another is for allergies, if both contain the same active ingredient-like acetaminophen or diphenhydramine-you’re doubling your dose. Always check the “Active Ingredients” section on the label before taking anything.
What if I only take one OTC medicine at a time? Am I still at risk?
Yes. The biggest risk comes from combining OTC meds with prescription drugs. For example, if you’re on a prescription painkiller that includes acetaminophen, taking Tylenol on the side-even once-can push you over the safe limit. Always check with your pharmacist before adding any new product.
Do herbal supplements count as medications?
Yes. Many herbal products contain active ingredients that interact with prescription drugs. St. John’s Wort can interfere with blood thinners. Kava can increase sedation when taken with sleep aids. And 68% of people don’t tell their doctors about these, making them hidden risks.
How often should I review my medications?
At least once a year-and every time you see a new doctor or start a new medication. If you’re taking five or more drugs, your pharmacist or primary care provider should do a full review every six months. Don’t wait for a problem to happen.
Can I trust the “Drug Facts” label on OTC products?
The FDA improved these labels in 2020, but a 2023 Government Accountability Office report found that 41% of people still can’t identify duplicate ingredients from them. Don’t assume it’s obvious. Read the “Active Ingredients” line carefully. If you’re unsure, ask your pharmacist.



13 Comments
Shannon Hale-17 November 2025
Let me just say this: if you’re still mixing cold meds with painkillers in 2025, you’re not just careless-you’re a walking liability. I’ve seen grandmas in the ER because they thought ‘natural’ meant ‘safe.’ Spoiler: St. John’s Wort + blood thinners = internal bleeding party. Stop trusting labels. Start trusting your pharmacist. And for god’s sake, stop pretending your vitamins don’t count as meds.
Eric Healy-19 November 2025
u/SHANNONHALE is right but also kinda overdramatic lol. i mean yeah double acetaminophen is bad but people dont just take 10 tylenol at once. its the slow drip over days that gets em. i took vicodin for a week then added advil cold cause i had a head cold. ended up with liver enzymes through the roof. no symptoms till i passed out at work. 3 days in the hospital. now i keep a spreadsheet. its weird but it works.
Jessica Healey-21 November 2025
My mom did this. Took NyQuil and her blood pressure med that had diphenhydramine in it. Slept for 18 hours straight. Woke up confused, couldn’t walk. Thought it was a stroke. Turned out it was just her brain being drowned in antihistamines. She’s fine now but she won’t touch OTC meds without checking the label first. I printed out a cheat sheet for her. It’s taped to her medicine cabinet. Small thing. Big difference.
Holli Yancey-23 November 2025
I appreciate the post. Really. But I think the real issue is how fragmented our healthcare system is. My dad sees four different specialists. Each one prescribes something. None talk to each other. He’s on 11 meds. The pharmacy flagged two overlaps, but only after he got hospitalized for a GI bleed from NSAID stacking. The system is broken. We can’t expect patients to be pharmacists.
Kelsey Robertson-23 November 2025
So let me get this straight-you want people to stop taking cold medicine because it might have the same ingredient as their painkiller? What about people who actually need both? Maybe the problem isn’t the meds-it’s the fear-mongering. I’ve been taking Tylenol and Sudafed together for 20 years. I’m fine. Maybe you’re just scared of chemistry.
Sridhar Suvarna-24 November 2025
India has similar issues. People buy 5 different brands of fever medicine because they think each one is stronger. No one checks the label. No one trusts the doctor. They trust the shopkeeper who says, ‘This one is for headache, that one for cold.’ The result? Liver failure in 40-year-olds. We need community health workers to go door to door with simple pictograms. Not apps. Not spreadsheets. Pictures.
saurabh lamba-26 November 2025
It's not about the pills, bro. It's about the illusion of control. We think we're managing our health... but we're just playing Russian roulette with our own biology. The real drug is ignorance. And it's legal. 😅
Gordon Mcdonough-27 November 2025
So I just got a new script for tramadol… and I checked my OTC stash… and guess what? I was already taking 3 things with acetaminophen… I didn’t even know!! I almost died. I’m gonna start carrying my med list like a passport. I printed it on cardstock. Laminated it. I’m not joking. My wife thinks I’m nuts. But I’m alive. So… yeah.
Levi Hobbs-29 November 2025
I work at a pharmacy. We catch maybe 1 in 4 double-dose cases. The rest? Patients say, ‘Oh, I didn’t think that counted.’ Or, ‘It’s just a little one.’ But ‘a little one’ adds up. I’ve seen 70-year-olds take 4 different nighttime meds-all with diphenhydramine. One of them died. I still think about it. Please. Just ask. Even if you think it’s dumb. Ask.
Joseph Peel- 1 December 2025
As someone who moved from the Philippines to the U.S., I was stunned by how many OTC meds contain the same ingredients. Back home, everything’s sold under one brand with clear warnings. Here? It’s a maze. I keep a notebook. I write down every pill I take. I show it to every new doctor. It’s a habit now. Simple. Effective. Doesn’t cost a dime.
Bill Machi- 1 December 2025
Stop pretending this is a healthcare issue. It’s a cultural one. Americans don’t want to be told what to do. They want to mix their own cocktails and then blame the system when it blows up. The FDA can’t fix stupidity. The only thing that saves people is a wake-up call from the ER. And even then, half of them go right back to doing the same thing. This isn’t education. It’s a battle against human nature.
henry mariono- 2 December 2025
I just started using Apple Health to log my meds. It flagged that my sleep aid had the same ingredient as my antidepressant. I didn’t even know they were connected. I’m not tech-savvy. But I’m alive. That’s enough.
Kiran Mandavkar- 2 December 2025
You’re all missing the point. The real danger isn’t the pills-it’s the belief that we can control complex biological systems with checklists and apps. Medicine isn’t a spreadsheet. It’s a dance with entropy. The only true safety is humility. And no app can teach you that.