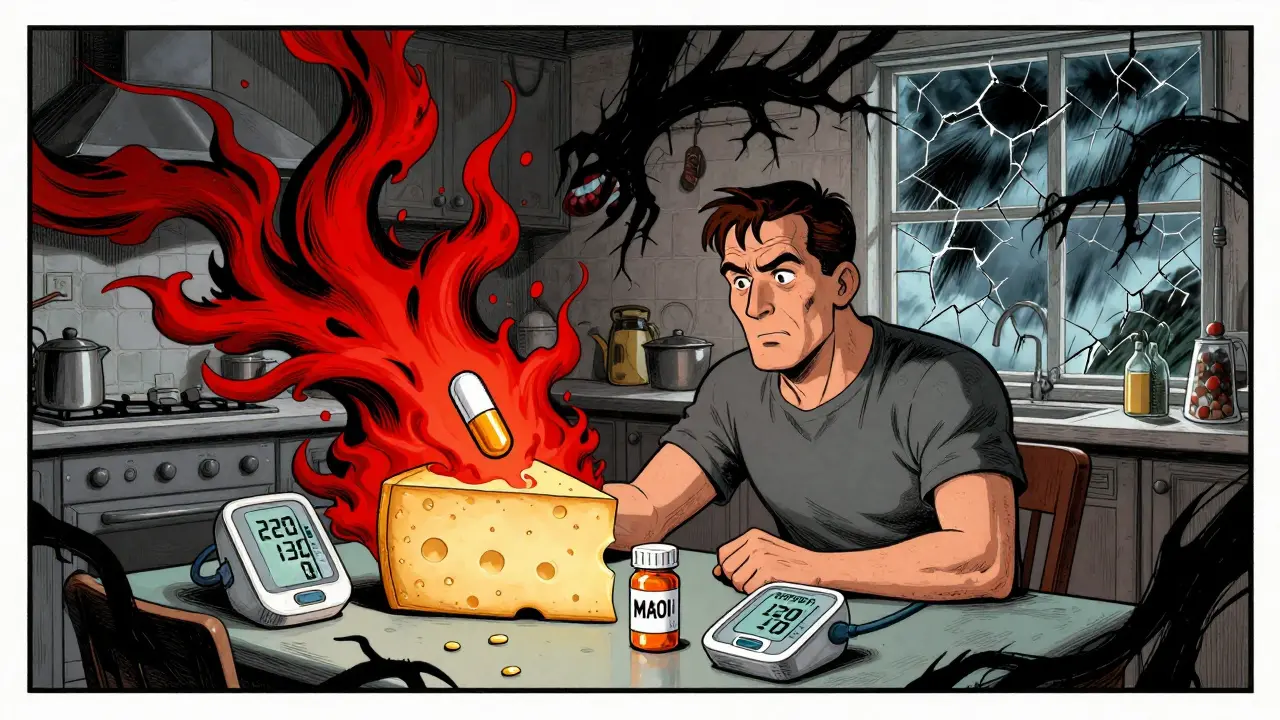
A severe hypertensive crisis isn’t just a bad day with a high blood pressure reading. It’s a medical emergency that can strike without warning - sometimes within minutes of taking a common medication or eating a harmless snack. Systolic pressure spikes above 180 mmHg, diastolic above 120 mmHg, and suddenly your brain, kidneys, heart, or eyes are under siege. This isn’t theoretical. People are ending up in the ICU because they didn’t realize their morning coffee with a decongestant, their new antidepressant, or even a piece of aged cheese could trigger a life-threatening reaction.
What Actually Triggers a Hypertensive Crisis?
Most people think high blood pressure is just about salt, stress, or genetics. But nearly one in five cases of sudden, dangerous hypertension comes from drugs - not just prescription pills, but over-the-counter meds, supplements, and even food. The real danger lies in drug interactions, where two or more substances combine in ways that shock the body’s blood pressure control system.
Take MAOIs, a class of antidepressants like phenelzine or selegiline. These drugs block an enzyme that breaks down norepinephrine - a natural stimulant. When you eat tyramine-rich foods like aged cheese, cured meats, or tap beer, tyramine floods your system, forcing norepinephrine out of storage. With MAOIs in the mix, there’s no way to clear it. The result? A surge in blood pressure. Case reports show systolic spikes over 220 mmHg in under an hour. One patient described waking up with 220/130 after eating cheddar with their selegiline - three days in the ICU, still terrified of cheese.
Then there’s venlafaxine. At doses above 300 mg/day, this common antidepressant can raise diastolic pressure past 90 mmHg. But here’s the kicker: doctors often miss it. Patients report headaches, dizziness, or blurred vision, and are told it’s just anxiety or aging. A review of 1,842 user reviews on Drugs.com found 42% said their concerns were dismissed - until their BP hit crisis levels.
Cocaine is another known trigger. But it’s the combo with beta-blockers like propranolol that’s deadly. Cocaine causes vasoconstriction. Propranolol blocks the heart’s response, leaving only the blood vessels to tighten unchecked. Systolic pressures above 220 mmHg aren’t rare in these cases. And it’s not just street drugs. Weight-loss pills, nasal decongestants like pseudoephedrine, and even some herbal stimulants can do the same thing - especially when mixed with antidepressants or blood pressure meds.
Hidden Culprits: Licorice, Cyclosporine, and Other Surprises
Most people don’t think of licorice candy as dangerous. But black licorice contains glycyrrhizin, which blocks the enzyme that protects your body from cortisol acting like a mineralocorticoid. That means your body starts retaining sodium, losing potassium, and holding onto fluid - all of which push blood pressure up. Patients have seen systolic pressure climb 30-40 mmHg after just a few weeks of daily licorice consumption. Blood tests show low potassium, high bicarbonate, and suppressed renin - classic signs of mineralocorticoid excess. The fix? Stop the candy. Blood pressure often drops back to normal in 10-14 days.
Transplant patients on cyclosporine face another hidden risk. Up to half of them develop hypertension within months. It’s not rejection - it’s the drug. Cyclosporine reduces sodium excretion and triggers vasoconstriction. Yet, in 55% of cases, doctors mistake it for organ rejection and increase immunosuppressants - making the hypertension worse. The fix? Switch to a calcium channel blocker like amlodipine. Studies show 78% effectiveness in controlling this type of crisis.
Even acetaminophen - the go-to pain reliever - can nudge BP up by 3-5 mmHg. It’s not enough to cause crisis alone, but in someone already on multiple meds, it’s the straw that breaks the camel’s back.

Why Doctors Miss It - And How You Can Protect Yourself
Here’s the uncomfortable truth: doctors don’t always ask about your meds. A multicenter study found only 35% of ER physicians routinely check for drug interactions in patients with severe hypertension. Why? Because the system isn’t built for it. Prescriptions come from different doctors. Patients take OTCs without telling anyone. Supplements are assumed to be safe. And labeling? Outdated. A 2022 JAMA analysis found 78% of high-risk medications lack clear warnings about hypertensive crisis - especially for off-label uses.
You can’t rely on your doctor to catch everything. You need to be your own advocate. Start with this simple checklist:
- Write down every pill, patch, drop, or supplement you take - including herbal teas and energy powders.
- Know your blood pressure. Check it at home weekly, especially if you’re on antidepressants, immunosuppressants, or stimulants.
- Ask: “Could any of these raise my blood pressure?” Don’t assume it’s safe just because it’s sold over the counter.
- Never mix MAOIs with decongestants, stimulants, or tyramine-rich foods. The FDA’s black box warning is there for a reason.
- If you’re on cyclosporine or similar drugs, insist on monthly BP checks and potassium tests.
Apps like ‘MAOI Diet Helper’ have helped 78% of users stick to safe diets in a Mayo Clinic trial. Use them. Set reminders. Share your list with every new provider - even the dentist.

What Happens in the ER - And What Works
If you’re in a hypertensive emergency, time is everything. The goal isn’t to bring pressure down fast - it’s to bring it down safely. Too rapid a drop can cause stroke or heart attack.
For MAOI-tyramine crises, intravenous phentolamine is the gold standard. It works in 20 minutes, with 92% success. Labetalol is also effective, especially if heart rate is racing. For cyclosporine-induced cases, calcium channel blockers like nifedipine or amlodipine are preferred. For stimulant-induced spikes, benzodiazepines help calm the nervous system while BP meds take effect.
But prevention beats emergency treatment every time. The FDA approved a new AI-driven decision-support tool in early 2023 that cuts MAOI-related emergencies by 40%. It flags risky combos in real time - if your EHR is connected. Ask your pharmacy or doctor if they use it.
The Bigger Picture: Why This Is Getting Worse
More people are on antidepressants than ever - prescriptions are growing 13% a year. Weight-loss drugs like phentermine are now widely available. Polypharmacy in older adults is rising. And many of these drugs aren’t tested together. The European Society of Cardiology found 18% of hypertensive emergencies in patients over 65 involve three or more interacting drugs.
By 2027, experts predict a 35% increase in drug-induced hypertensive crises. The cost? $2.3 billion a year in avoidable ER visits and hospital stays. The fix isn’t just better drugs - it’s better communication. Better labeling. Better systems. But until then, your awareness is the best defense.
Know your meds. Know your numbers. Ask the hard questions. A severe hypertensive crisis can come from something as simple as a candy bar and a pill - and it doesn’t have to happen to you.
Can over-the-counter cold medicine cause a hypertensive crisis?
Yes. Decongestants like pseudoephedrine and phenylephrine are strong vasoconstrictors. When taken with MAOIs, SSRIs, or even some blood pressure medications, they can trigger a sudden spike in blood pressure - sometimes over 200 mmHg systolic. Even if you don’t have high blood pressure, these combinations can push you into crisis. Always check labels and ask your pharmacist before using OTC cold meds if you’re on antidepressants or other chronic meds.
Is it safe to eat cheese while on MAOIs?
No. Aged cheeses (like cheddar, parmesan, blue cheese), cured meats, tap beer, soy sauce, and fermented foods contain tyramine. When MAOIs are active in your system, tyramine causes a massive release of norepinephrine, leading to a hypertensive emergency. Even small amounts can trigger a crisis. The FDA requires black box warnings on MAOI labels for this reason. If you’re on an MAOI, avoid these foods completely - not just occasionally.
How long should I wait between stopping an MAOI and starting another antidepressant?
The American Heart Association recommends a 2-week washout period for reversible MAOIs like moclobemide. For irreversible ones like phenelzine or tranylcypromine, wait 4-5 weeks. This is critical - serotonin syndrome and hypertensive crisis can both occur if you start an SSRI or SNRI too soon. Never switch antidepressants without clear guidance from your doctor. Even a few days too soon can be dangerous.
Can licorice candy really raise my blood pressure?
Yes - and it’s not just a myth. Black licorice contains glycyrrhizin, which mimics aldosterone, causing your body to hold onto sodium and lose potassium. This leads to fluid retention and elevated BP. In some cases, systolic pressure rises 30-40 mmHg within weeks. Blood tests show low potassium, high bicarbonate, and suppressed renin. Stopping licorice usually reverses the effect within 10-14 days. Red licorice or licorice-flavored candy without glycyrrhizin is safe.
What should I do if I think I’m having a hypertensive crisis?
If your blood pressure is over 180/120 and you have symptoms like severe headache, chest pain, shortness of breath, blurred vision, or confusion - call 911 immediately. Do not wait. Do not try to drive yourself. This is not a situation to manage at home. Even if you feel fine, a pressure this high can cause silent organ damage. Emergency teams will use IV medications to lower pressure safely. Your survival depends on quick action.
Are newer antidepressants safer than older ones?
Not necessarily. While SSRIs like fluoxetine are generally safer than MAOIs, venlafaxine (an SNRI) carries a significant risk at doses above 225 mg/day. The American College of Cardiology now classifies venlafaxine above this dose as “high risk” for hypertension. Even sertraline and escitalopram can interact with decongestants or stimulants. No antidepressant is risk-free when combined with other drugs. The key isn’t the class - it’s the combination and dosage. Always review your full medication list with your prescriber.
Next steps: If you’re on any medication listed here, talk to your doctor about your BP monitoring plan. Ask if your pharmacy uses a drug interaction checker. Keep a printed list of your meds in your wallet. And if you’ve ever had unexplained high blood pressure - especially after starting a new drug - don’t brush it off. It might have been a warning sign.




8 Comments
Matthew Hekmatniaz- 1 January 2026
Just read this and had to pause. I’m on an MAOI and honestly thought the cheese warning was exaggerated until my buddy had a seizure after a plate of blue cheese and a cold pill. Now I carry a card in my wallet that says ‘MAOI USER - NO TYRAMINE.’ It’s weird, but it’s saved me from three near-misses at restaurants. If you’re on these meds, don’t wing it. This isn’t just ‘eat healthy’ stuff-it’s life or death.
Liam George- 2 January 2026
They don’t want you to know this, but the FDA and Big Pharma are deliberately downplaying drug interactions because if people realized how many meds are ticking time bombs, they’d stop taking them. MAOIs? A 1950s relic they kept around for profit. Licorice? A natural remedy they turned into a villain because it can’t be patented. The real crisis isn’t the drugs-it’s the system that profits from your ignorance. Ask yourself: why do they bury this info in 12,000-word medical journals and not on the bottle?
sharad vyas- 2 January 2026
My uncle in India was on cyclosporine after transplant. He ate too much salty pickle and his BP shot up. Doctors thought it was rejection. Took three weeks to figure out it was the salt and the drug. Now he eats only fresh food, checks BP every day, and says, ‘My body is a temple, not a lab experiment.’ Simple advice. But true.
Dusty Weeks- 3 January 2026
just took a decongestant last week and felt like my head was going to explode 💥😭 why does no one tell you this stuff???
Sally Denham-Vaughan- 4 January 2026
OMG this is so real. My sister was on venlafaxine and started taking those ‘natural energy boosters’ from the health store. She ended up in the ER with a 210/125 reading. The ER doc was like, ‘Did you take anything else?’ She said, ‘Just the green powder.’ He sighed and said, ‘That’s your problem.’ I made her delete every supplement app and only use pharmacy-approved stuff. Seriously, if you’re on meds, don’t trust influencers with ‘superfoods.’
Ann Romine- 5 January 2026
I’ve been on SSRIs for years and never realized how many OTC meds interact. I used to take Sudafed for allergies without a second thought. After reading this, I went through my medicine cabinet and found three items that could’ve triggered something. I’ve since started using the ‘MAOI Diet Helper’ app-it’s clunky, but it saved me from accidentally buying licorice-flavored gum. Small habits matter.
Todd Nickel- 6 January 2026
The systemic failure here is not just individual ignorance but the fragmentation of medical data. Patients receive prescriptions from three different providers, buy supplements from three different retailers, and none of those systems communicate. The AI tool mentioned is a step forward, but it’s useless if your pharmacy uses a 2015 EHR and your psychiatrist uses a 2022 platform. Until interoperability becomes mandatory-not optional-this will keep happening. We need federal regulation of drug interaction databases, standardized labeling across all OTC products, and mandatory pharmacist counseling for high-risk combinations. This isn’t just about awareness-it’s about infrastructure.
Alex Warden- 6 January 2026
People are dying because they’re too lazy to read labels. If you’re taking pills, you owe it to yourself to know what’s in them. No one’s holding your hand. Stop blaming the system and start taking responsibility. This isn’t a conspiracy-it’s basic adulting. If you can’t manage your meds, don’t complain when you end up in the ICU.