Many people take statins without ever questioning if they still need them. These drugs, prescribed to lower cholesterol and prevent heart attacks or strokes, are among the most common medications in the world. But for some - especially older adults or those with serious health conditions - continuing statins may do more harm than good. The real question isn’t whether statins work. It’s: when should you stop? And how do you do it without putting your heart at risk?
Why Do People Stop Statins?
About 1 in 5 people who start statins stop taking them for at least a year. The biggest reason? Side effects. Muscle pain, weakness, or cramps are the most common complaints. Some people worry about developing type 2 diabetes, liver issues, or memory problems. Others just feel tired of taking a daily pill for the rest of their life - especially if they’ve never had a heart attack or stroke. But here’s the catch: many of these side effects aren’t actually caused by statins. Studies show that when patients who stopped statins due to muscle pain were put on a placebo, nearly 90% of them still reported the same symptoms. That means their pain wasn’t from the drug - it was from aging, inactivity, or another condition. Still, fear is powerful. And once someone stops, they often don’t go back.Who Should Consider Stopping Statins?
Not everyone who takes statins needs to keep taking them forever. There are clear situations where stopping makes sense. 1. Limited life expectancyIf you have a serious illness like advanced cancer, severe heart failure, or dementia with a life expectancy of less than two years, continuing statins offers little to no benefit. In fact, the American Geriatrics Society and other experts now say it’s often better to stop. Why? Because you’re not going to live long enough to see the long-term heart benefits. But you’ll still feel the side effects - muscle aches, fatigue, digestive issues. Stopping can improve quality of life in the final months or years. 2. Primary prevention in older adults
If you’ve never had a heart attack, stroke, or blocked artery - and you’re over 75 - the benefit of statins drops sharply. A 2021 study found that for every 112 people over 75 who stopped statins for primary prevention, one extra heart attack or stroke happened per year. That’s a small risk. But for someone with multiple health problems, frailty, or limited mobility, that small risk might not outweigh the daily burden of the pill. 3. Severe side effects that don’t improve
If you’ve tried switching to a different statin, lowering the dose, or taking it every other day - and your muscle pain or weakness still won’t go away - continuing may not be worth it. Some people just can’t tolerate them, no matter what. In those cases, the focus shifts to other ways to protect the heart.
What Happens When You Stop?
Stopping statins doesn’t mean your cholesterol instantly spikes back to dangerous levels. It takes weeks or even months for LDL (bad cholesterol) to rise significantly. But here’s the important part: if you’re at high risk for heart disease, stopping means your risk starts climbing again. For people who’ve already had a heart attack or stroke (secondary prevention), stopping statins increases the chance of another major event. The same 2021 study found that for every 77 people who stopped, one extra heart attack, stroke, or death occurred each year. That’s a big deal. But for older adults with no prior heart disease, the risk is much lower. A 2024 review of end-of-life patients found no increase in death rates after stopping statins - even in those who had recently had a heart attack. If someone is in hospice care with only days or weeks to live, continuing statins adds no meaningful benefit. It just adds more pills to the pile.
How to Stop Safely
Never just quit cold turkey without talking to your doctor. Even if you’re sure you want to stop, you need a plan.- Have a real conversation - Ask: “What’s my risk of a heart event if I stop? What’s my risk of side effects if I keep going?” Don’t accept vague answers. Request numbers. Ask for your 10-year risk score if you have one.
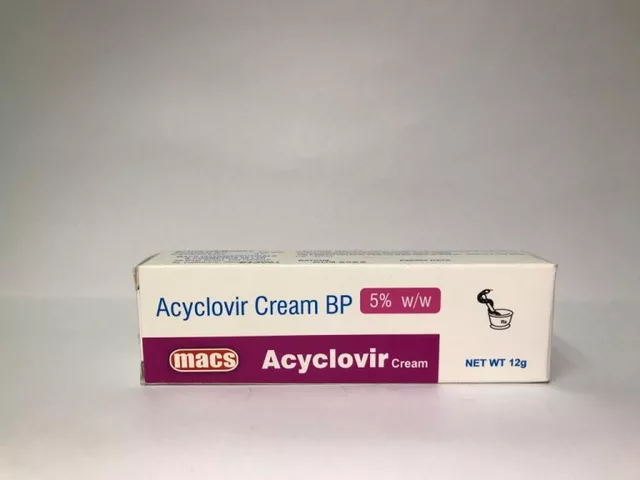
- Try alternatives first - If side effects are the problem, your doctor might suggest a lower dose, a different statin (like pravastatin or fluvastatin, which are gentler), or taking it every other day. Some people tolerate intermittent dosing better.
- Consider non-statin options - If you can’t take statins but still need cholesterol control, ezetimibe or PCSK9 inhibitors are options. But they’re expensive. Fibrates and omega-3s help a little, but they don’t cut heart risk like statins do.
- Monitor after stopping - Get your cholesterol checked 6 to 8 weeks after stopping. If your LDL shoots up above 190 mg/dL, you may need to reconsider.
- Document why you stopped - Too often, doctors just check “no longer necessary” in the chart. That hides the real reason - muscle pain, fear, or poor quality of life. Make sure your reason is clearly recorded.
What About Natural Alternatives?
You’ll hear a lot about red yeast rice, garlic, plant sterols, or niacin as “natural statins.” But here’s the truth: red yeast rice contains the same active ingredient as lovastatin - and it’s not regulated. You don’t know the dose. You don’t know if it’s safe. It can cause the same side effects as prescription statins, with no oversight. Plant sterols and soluble fiber (like oats, beans, and psyllium) can lower LDL by 5-10%. That’s helpful - but not enough if you’re high risk. Exercise, quitting smoking, and eating less processed food matter more than any supplement.Who Should NEVER Stop Statins?
Some people absolutely should not stop without strong medical advice:- Those who’ve had a heart attack, stroke, or stent placement
- People with diabetes and other risk factors (high blood pressure, smoking, family history)
- Anyone with very high LDL (over 190 mg/dL) without other clear causes
- Patients under 75 with multiple risk factors and a 10-year risk above 20%

The Bigger Picture: Deprescribing Is Part of Good Care
We’ve been trained to think that more pills = better care. But that’s not true. Taking too many drugs - especially when you’re older and sicker - increases falls, confusion, hospital stays, and death. Statins are just one part of that. Experts now call this “deprescribing” - the thoughtful, planned reduction of medications that no longer help. It’s not giving up. It’s choosing quality of life over abstract long-term numbers. A 2023 study in Switzerland, France, and the Netherlands is following 1,800 older adults with multiple health problems to see if stopping statins is safe. The results, expected in late 2025, could change how we treat thousands.Final Thoughts
Statins save lives - but they’re not for everyone, forever. If you’re taking one and wondering whether you still need it, ask your doctor these questions:- What’s my real risk of heart disease right now?
- What’s my life expectancy? Do I have a serious illness?
- Am I taking this pill because it helps me - or because I’ve always taken it?
- Can we try lowering the dose or switching first?
Can I stop statins cold turkey?
Technically, yes - but it’s not recommended. Stopping suddenly doesn’t cause immediate danger, but it removes your protection against heart events. If you’re high risk, your cholesterol can rise quickly. Always talk to your doctor first. They may suggest tapering or switching to a lower dose before stopping completely.
Do statins cause muscle damage?
Rarely. True muscle damage (rhabdomyolysis) happens in fewer than 1 in 10,000 people. More commonly, people feel general muscle aches or weakness. Studies show that in many cases, the pain isn’t from the statin at all - it’s from aging, arthritis, or lack of activity. A doctor can check your CK levels to rule out real damage.
Will my cholesterol go back up if I stop?
Yes - usually within 4 to 8 weeks. Statins work by blocking cholesterol production. When you stop, your liver goes back to making it normally. How high it rises depends on your genetics, diet, and baseline risk. A blood test after stopping will show you the change.
Are there natural ways to lower cholesterol without statins?
Yes - but they’re not as powerful. Eating more oats, beans, nuts, and fiber can lower LDL by 5-10%. Regular exercise, losing weight, and quitting smoking help too. But if you’re at high risk for heart disease, these alone won’t reduce your risk enough. Statins are still the most effective tool we have for high-risk people.
What if I stop statins and have a heart attack?
If you stopped without medical advice and were at high risk, you may have increased your chances. But that doesn’t mean stopping was always wrong. For some people - especially those with limited life expectancy or severe side effects - the benefits didn’t justify the risks. The key is making the decision together with your doctor, based on your individual situation - not fear or assumptions.
Is it safe to stop statins if I’m over 80?
It can be - if you’re healthy and active, no. But if you’re frail, have multiple chronic illnesses, or a life expectancy under two years, stopping is often the safer, more compassionate choice. The 2023 American Geriatrics Society guidelines support deprescribing statins in older adults with poor health status. Age alone isn’t the reason - your overall health is.
Next Steps
If you’re thinking about stopping statins:- Check your latest cholesterol and heart risk score.
- Write down why you want to stop - side effects? Fatigue? Fear?
- Ask your doctor: “What’s my 10-year risk? What happens if I stop?”
- Ask if you can try a lower dose or different statin first.
- Get your cholesterol tested 6 weeks after stopping.
- Keep monitoring your health - if you feel chest pain, dizziness, or shortness of breath, get checked immediately.



12 Comments
Andrew Forthmuller-14 November 2025
Statins? Nah, I stopped last year. No muscle pain, just felt better without the pill.
dace yates-14 November 2025
I’ve been on statins for 8 years. Never had a heart issue, but my doctor said ‘just in case.’ Now I’m 78, diabetic, and my knees hurt worse than my cholesterol. I asked if I could stop - she said ‘let’s try lowering the dose first.’ I’m still taking half, but I sleep better. No more that icky fatigue.
Danae Miley-14 November 2025
Let’s be clear: the 90% placebo effect on muscle pain is not a fluke - it’s a well-documented phenomenon in multiple randomized controlled trials. The medical community needs to stop blaming statins for every ache in older adults. It’s not the drug; it’s the aging process, sarcopenia, and sedentary lifestyles. We’re overmedicalizing normal human decline.
Renee Ruth-15 November 2025
My uncle stopped his statin because he ‘felt weird.’ Three months later, he had a stroke. Now he can’t talk. His wife says he was ‘just tired of pills.’ But what if he’d listened to his cardiologist? Now he’s in a nursing home. I’m not saying statins are perfect - but I’m not taking chances with my heart. Not after that.
Charles Lewis-16 November 2025
It is imperative that we recognize the ethical and clinical nuances surrounding deprescribing in geriatric populations. While statins have demonstrated unequivocal benefit in secondary prevention, their utility in primary prevention among the frail elderly - particularly those with multimorbidity and limited life expectancy - is increasingly called into question by contemporary guidelines from the American College of Cardiology and the American Geriatrics Society. The burden of polypharmacy, compounded by potential adverse effects such as myopathy, cognitive fog, and gastrointestinal distress, may outweigh the marginal gains in absolute risk reduction. Therefore, a patient-centered, individualized approach - one that prioritizes quality of life, functional status, and patient autonomy - must supplant the default assumption of lifelong pharmacotherapy. We must not confuse adherence with beneficence.
Samantha Wade-17 November 2025
People think stopping statins is just ‘going natural’ - but if you’ve had a stent or a heart attack, you’re not just ‘taking a pill’ - you’re maintaining a lifeline. I work in cardiology. I’ve seen too many patients come in after stopping because ‘they felt fine’ - and then they’re back in the ER with a blocked artery. The data doesn’t lie: for high-risk patients, statins are non-negotiable. If side effects are an issue, there are alternatives - lower doses, different statins, ezetimibe. But don’t quit cold turkey and call it ‘self-care.’ That’s not bravery - it’s dangerous ignorance.
Elizabeth Buján-19 November 2025
i just wanna say… i stopped mine last year after my grandma died. she was 92, took 12 pills a day, and still said she felt ‘like a ghost.’ i didn’t want that. i’m 76, active, walk 5 miles a week, eat veggies, no heart problems. my doc said ‘your risk is low.’ so i stopped. no muscle pain, no weird dreams, no more panic about my numbers. i feel more alive than i have in years. maybe it’s not about the cholesterol… maybe it’s about living.
vanessa k-20 November 2025
I get both sides. My mom’s on statins and hates them - says they make her tired and her legs cramp. But she’s 81, had a stent in 2018, and her LDL is still 160. I told her to talk to her doctor about switching to a lower dose or trying ezetimibe. She’s scared to stop, but also scared to keep taking it. I think the real issue isn’t the drug - it’s that we don’t have enough honest conversations about what ‘quality of life’ means when you’re older. No one talks about the emotional toll of taking pills you don’t want.
manish kumar-22 November 2025
In India, many elderly patients are prescribed statins automatically - even when they have no cardiovascular history. The cultural belief is that ‘if the doctor says it, you take it.’ But I’ve seen cases where patients stop statins and live longer, healthier lives because they finally stopped being medicated into submission. The real problem isn’t statins - it’s the medical system that treats aging as a disease to be managed with pills. We need more education, not more prescriptions. I’ve encouraged my own father to get his 10-year risk score - he was shocked to learn he was under 5%. He’s not stopping yet, but he’s asking questions. That’s progress.
Nicole M-23 November 2025
My mom’s 79 and has been on statins since 2010. She’s never had a heart problem. She just took it because her doctor said ‘everyone over 65 should.’ She finally asked why and the answer was ‘it’s just standard.’ That made me furious. She’s active, eats clean, walks every day. Her cholesterol is high but stable. We got a second opinion - the new doc said ‘you can stop, monitor, and see.’ She did. No crash. No disaster. Just… life. I think we need to stop treating older people like ticking time bombs.
Arpita Shukla-23 November 2025
Red yeast rice is not a ‘natural alternative’ - it’s unregulated lovastatin. The FDA has warned about it multiple times. People think ‘natural’ means safe - but that’s a myth. Also, if you’re over 75 and have diabetes, stopping statins is a terrible idea unless you have a life expectancy under 2 years. The 2021 study you cited? It was observational, not randomized. And the 2024 end-of-life review? That was hospice patients - not healthy 80-year-olds. Don’t cherry-pick studies to justify laziness.
Benjamin Stöffler-24 November 2025
Let’s not pretend this is about ‘quality of life’ - it’s about fear. Fear of aging. Fear of mortality. Fear of being told you’re not invincible. Statins are not the enemy. The enemy is the cultural delusion that we can outrun biology with willpower, supplements, and denial. The liver doesn’t care how ‘natural’ you feel. The arteries don’t care if you ‘feel better’ without pills. And if you’re high-risk - and you stop - you’re not being ‘smart,’ you’re being statistically reckless. The numbers don’t lie. The data doesn’t care about your feelings. Your cholesterol? It’s not a metaphor. It’s a number. And if it’s high - and you’re high-risk - it’s going to kill you. No amount of ‘I feel better’ changes that.