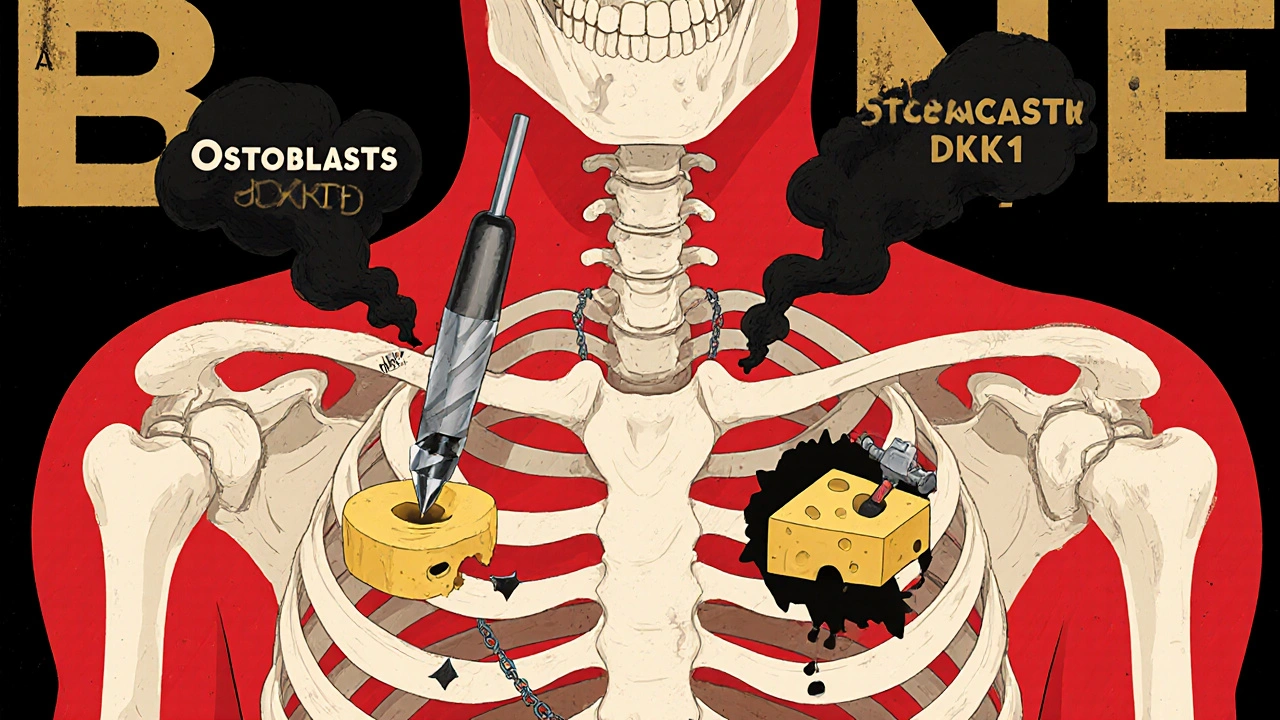
Bone Disease: Causes, Symptoms, and How Medications Help
When you hear bone disease, a group of conditions that weaken or damage the skeletal system. Also known as skeletal disorder, it isn’t just about aging—it can start early, show up without warning, and quietly steal your mobility. Think of your bones like a building: if the foundation cracks or the support beams rust, everything else starts to sag. That’s what happens in osteoporosis, a condition where bones become porous and fragile, or in osteoarthritis, where the cushion between joints breaks down. These aren’t just "old person problems." They show up in people in their 40s and 50s, especially if they’ve had long-term steroid use, poor nutrition, or chronic inflammation.
Bone disease often hides behind something more obvious: pain. Not the kind that goes away after a few days, but the deep, constant ache that makes walking, standing, or even sleeping hard. That pain isn’t always from injury—it’s from your bones losing density, your cartilage wearing thin, or nerves getting irritated by misaligned joints. Many people mistake it for general aging or muscle strain. But when pain lasts beyond healing, or spreads without a clear cause, it could be central sensitization, a nervous system glitch that turns normal signals into intense pain. That’s why some with bone disease feel pain everywhere, even when scans look normal. And yes, medications play a big role—not just to numb the pain, but to slow the damage. Drugs like bisphosphonates for osteoporosis, or NSAIDs for joint inflammation, are common. But they come with risks. Taking too much ibuprofen for bone pain? That can hurt your stomach or kidneys. Mixing it with other meds? You might accidentally double up on ingredients, like acetaminophen, and overdose without knowing it.
Managing bone disease isn’t just about popping pills. It’s about knowing when to stop, when to switch, and how to protect yourself from side effects. That’s why deprescribing—safely cutting back on unnecessary meds—is becoming a key part of care. It’s also why safe storage matters: if kids or pets get into your bone meds, the results can be deadly. And while some treatments focus on bones alone, others protect your whole body. For example, if you’re on statins for heart health, you might be lowering your bone turnover too. Or if you’re on beta-blockers for blood pressure, you might not feel your blood sugar drop—something that can worsen nerve damage linked to bone pain. The posts below give you real, no-fluff answers: how to spot early signs, which meds actually work, what to avoid, and how to talk to your doctor without getting lost in jargon. You’ll find guides on switching meds safely, avoiding dangerous drug combos, and understanding why some treatments fail. This isn’t theory. It’s what people are using right now to move better, feel less pain, and stay in control.
Multiple Myeloma: Understanding Bone Disease and the New Drugs Changing Outcomes
Multiple myeloma causes severe bone damage in over 80% of patients. Learn how new drugs are shifting from preventing bone loss to actually healing bones, and what patients should do now.