CAR T-cell therapy: What it is, how it works, and what patients need to know
When you hear CAR T-cell therapy, a type of personalized cancer treatment that reprograms a patient’s own immune cells to attack tumors. Also known as chimeric antigen receptor T-cell therapy, it’s not a drug you swallow—it’s a living treatment made from your blood. This isn’t science fiction. Since the first FDA approvals in 2017, it’s helped people with advanced leukemia, lymphoma, and multiple myeloma who ran out of other options.
Here’s how it works in simple terms: Doctors pull out your T-cells—the immune system’s frontline fighters—and send them to a lab. There, scientists give them a new targeting system, like a GPS for cancer cells. These modified cells, now called CAR T-cells, are multiplied in the thousands, then put back into your body. Once inside, they hunt down and destroy cancer cells that match their target. It’s like upgrading your body’s defense system with custom-made soldiers.
This treatment is powerful, but it’s not for everyone. It’s mostly used for blood cancers that haven’t responded to chemo or radiation. It’s also expensive, complex, and comes with serious risks. Some patients develop cytokine release syndrome—a dangerous immune overreaction—or neurological side effects like confusion or seizures. That’s why it’s only done at specialized centers with teams trained to handle these emergencies.
Related to CAR T-cell therapy are cancer immunotherapy, a broad category of treatments that boost the body’s natural ability to fight cancer, which includes checkpoint inhibitors and vaccines. But CAR T-cells are different—they’re engineered, not just activated. They’re also connected to T-cell engineering, the science of modifying immune cells to better target disease, which is now being tested for solid tumors like lung and pancreatic cancer. And while CAR T-cells are often discussed alongside blood cancer treatment, therapies focused on leukemias, lymphomas, and myelomas, their real breakthrough is proving that the immune system can be rewired to beat cancer, even when it’s advanced.
What you’ll find in the posts below isn’t just theory. These are real stories about how people manage side effects, what recovery looks like, and how this treatment fits into the bigger picture of cancer care. You’ll see how it connects to medication safety, patient protection laws, and the growing role of personalized medicine. There’s no sugarcoating—it’s intense, expensive, and not always successful. But for some, it’s the only thing that worked.
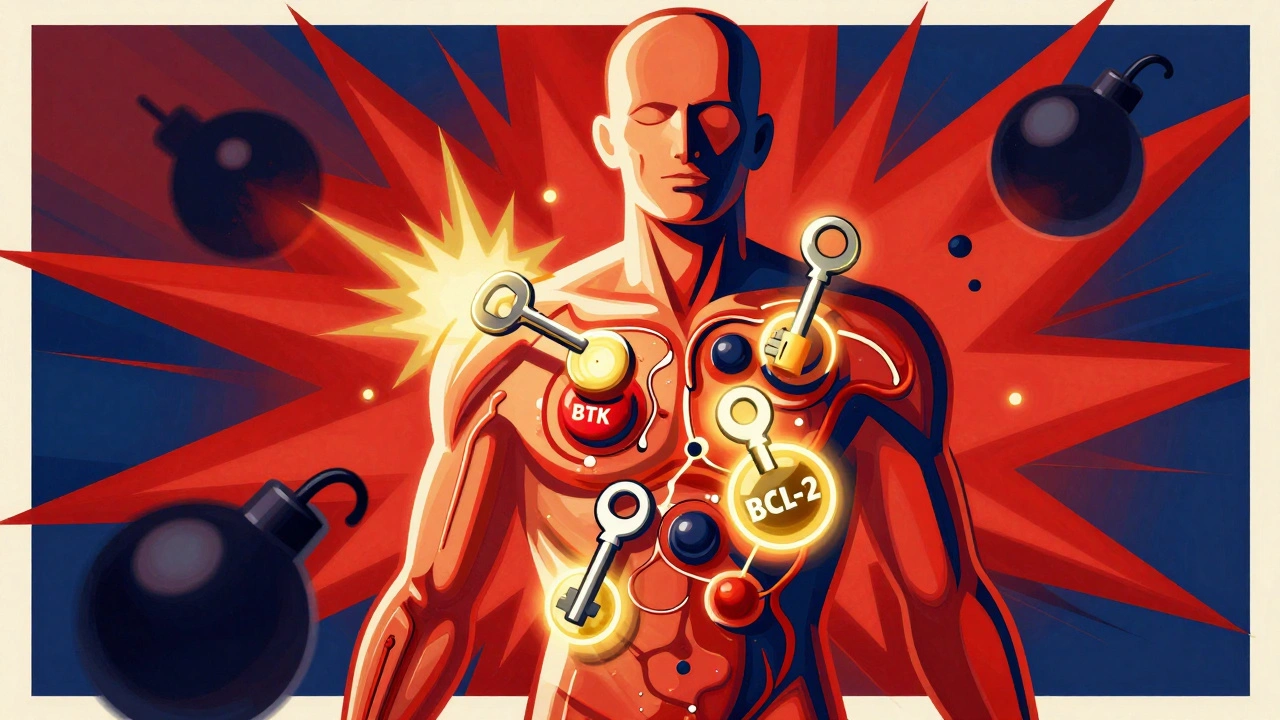
Leukemia and Lymphoma: How Targeted and Cellular Therapies Are Changing Survival Rates
Targeted and cellular therapies are transforming leukemia and lymphoma treatment, offering longer remissions and even cures where chemotherapy failed. Learn how drugs like venetoclax and CAR T-cell therapy work-and who benefits most.