Cellular Therapy: What It Is, How It Works, and What You Need to Know
When you hear cellular therapy, a medical treatment that uses living cells to repair, replace, or regenerate damaged tissues or immune responses. Also known as cell-based therapy, it’s not science fiction—it’s already helping people with cancers, autoimmune disorders, and degenerative conditions. Unlike pills or surgery, cellular therapy works by introducing live cells into your body to fix problems at the source. These cells can be your own, donated, or even engineered in a lab to target specific diseases.
This approach is part of a bigger field called regenerative medicine, a branch of healthcare focused on restoring or replacing damaged organs and tissues. It includes stem cell treatment, using unspecialized cells that can turn into different types of body cells, and immunotherapy, a type of cellular therapy that boosts your immune system to fight cancer or chronic infections. These aren’t just experimental anymore. Some forms are FDA-approved, covered by insurance, and used in hospitals daily.
But not all cellular therapies are created equal. Some are backed by decades of research, like CAR-T cell therapy for certain blood cancers. Others are offered by clinics with little proof, preying on hope. That’s why knowing the difference matters. You need to understand what’s real, what’s promising, and what’s risky. The posts below break down real cases—how patients responded, what side effects showed up, and which treatments actually delivered results. You’ll find guides on how to spot legitimate providers, what questions to ask your doctor, and how insurance handles these treatments. No fluff. No hype. Just what works, what doesn’t, and what you need to know before you consider it.
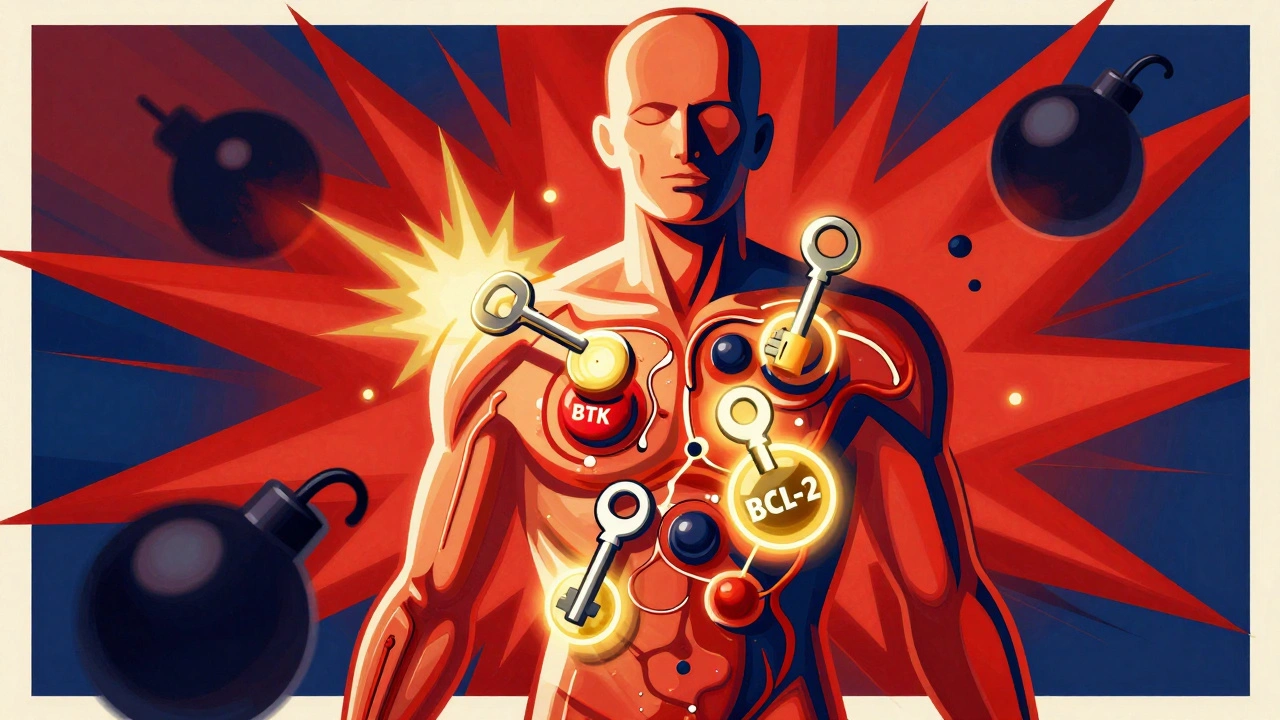
Leukemia and Lymphoma: How Targeted and Cellular Therapies Are Changing Survival Rates
Targeted and cellular therapies are transforming leukemia and lymphoma treatment, offering longer remissions and even cures where chemotherapy failed. Learn how drugs like venetoclax and CAR T-cell therapy work-and who benefits most.