Leukemia Treatment: Options, Side Effects, and What Works Today
When someone is diagnosed with leukemia, a type of blood cancer that starts in the bone marrow and floods the bloodstream with abnormal white blood cells. Also known as blood cancer, it doesn’t affect everyone the same way — some forms grow slowly, others need immediate action. The good news? Treatment has changed a lot in the last decade. What used to mean months in the hospital and brutal chemo is now often a mix of pills, targeted drugs, and shorter stays — with better survival rates than ever before.
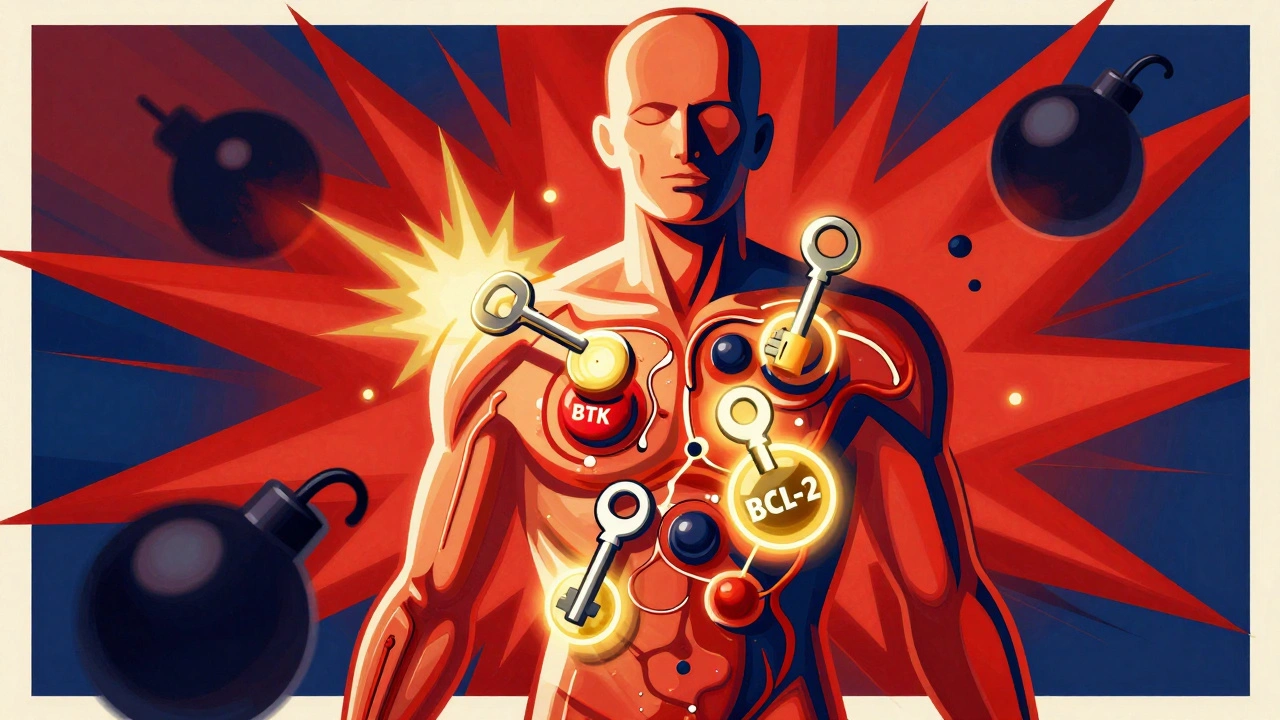
Not all chemotherapy for leukemia, the traditional backbone of treatment that kills fast-growing cells, both cancerous and healthy is the same anymore. Doctors now pick drugs based on the exact type of leukemia — acute lymphoblastic (ALL), acute myeloid (AML), chronic lymphocytic (CLL), or chronic myeloid (CML). For example, someone with CML might start on a daily pill like imatinib instead of IV chemo. These targeted therapy, drugs designed to attack specific mutations in cancer cells without wrecking the whole body have fewer side effects and often work better than old-school chemo. And when chemo is needed, it’s usually shorter, more precise, and paired with drugs that protect healthy cells.
For some patients, especially younger ones with aggressive forms, a stem cell transplant, a procedure that replaces damaged bone marrow with healthy donor cells to rebuild the immune system is still the best shot at a cure. But it’s not for everyone — it’s risky, requires a matched donor, and leaves you vulnerable to infections for months. That’s why doctors now use it more selectively, often after targeted therapy has shrunk the cancer first. Meanwhile, newer options like CAR T-cell therapy — where your own immune cells are trained to hunt leukemia — are helping people who didn’t respond to anything else.
Side effects still happen — fatigue, nausea, low blood counts, increased infection risk — but they’re better managed now. Blood transfusions, growth factors, and antibiotics are part of the routine. Many patients also use CGMs or regular blood tests to catch drops in white cells early. And because treatment is so personalized, your doctor will adjust based on your age, overall health, and even your genes. There’s no one-size-fits-all plan anymore.
What you’ll find in the posts below are real-world insights from people managing leukemia treatment — how to handle side effects, what to ask your oncologist, why some meds work better than others, and how to stay safe when your immune system is down. You’ll see how drugs like clozapine can trigger dangerous drops in white blood cells, why medication adherence matters even when you feel fine, and how automated refills help patients stick to complex regimens. This isn’t just theory — it’s what people are living through every day, and what works for them.
Leukemia and Lymphoma: How Targeted and Cellular Therapies Are Changing Survival Rates
Targeted and cellular therapies are transforming leukemia and lymphoma treatment, offering longer remissions and even cures where chemotherapy failed. Learn how drugs like venetoclax and CAR T-cell therapy work-and who benefits most.