Every year, thousands of older adults end up in the hospital because of a medication that shouldn’t have been prescribed in the first place. It’s not always a mistake - sometimes it’s just how medicine has been done for decades. But the Beers Criteria are changing that. They’re not a law. They’re not a blacklist. They’re a clear, evidence-based guide to help doctors and pharmacists avoid drugs that do more harm than good in people over 65.
What Exactly Are the Beers Criteria?
The Beers Criteria are a list of medications that experts agree should be avoided or used with extreme caution in older adults. First created in 1991 by Dr. Mark Beers, they’re now maintained and updated every few years by the American Geriatrics Society (AGS). The latest version came out in 2023, after reviewing over 1,500 new studies.It’s not just about naming bad drugs. It’s about understanding why they’re risky. As we age, our bodies change. The liver slows down. The kidneys don’t filter as well. Fat and muscle ratios shift. That means a drug that’s safe for a 40-year-old can build up to toxic levels in a 75-year-old. Even common over-the-counter pills - like diphenhydramine in Benadryl - can cause confusion, falls, or urinary retention in older people.
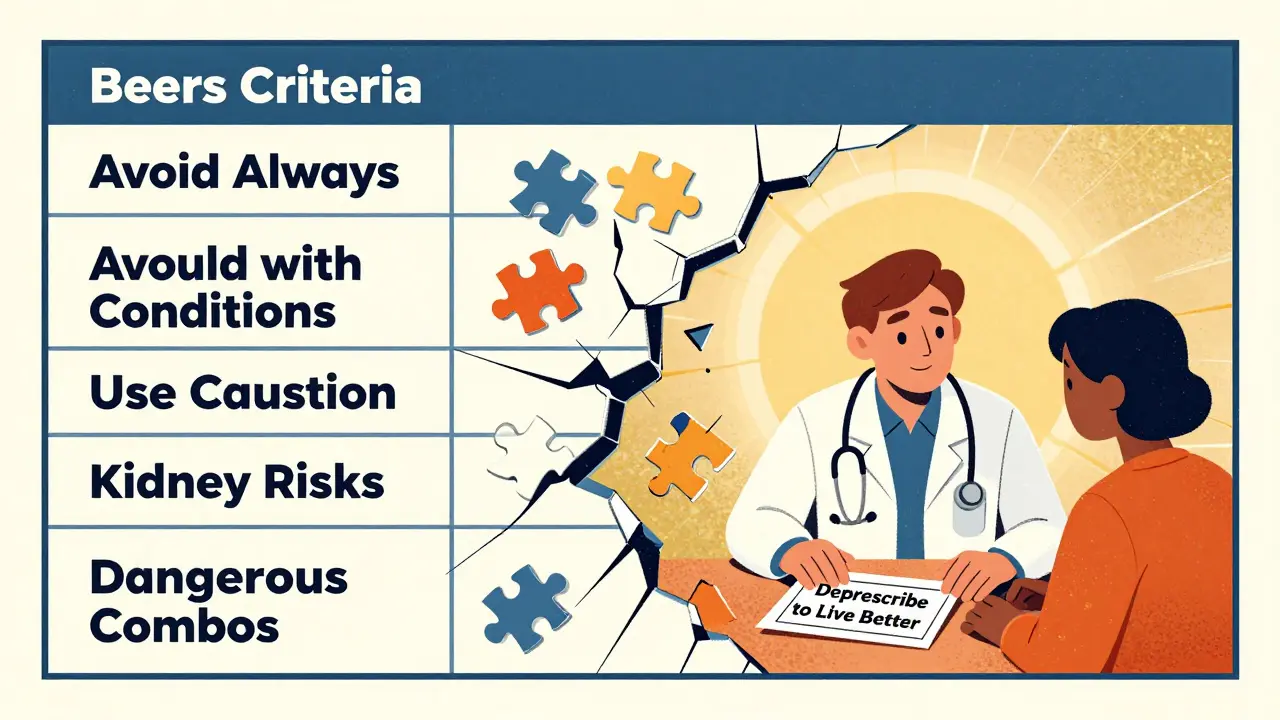
The 2023 update includes 131 specific medication criteria. That’s not a small list. It’s broken into five clear sections:
- Drugs to avoid in most older adults - no matter what else is going on
- Drugs to avoid if you have certain conditions - like heart failure, dementia, or prostate problems
- Drugs to use with caution - they’re not always dangerous, but they need close monitoring
- Drugs to avoid if kidney function is reduced
- Drug combinations that create dangerous interactions
For example, the list now strongly warns against antipsychotics like haloperidol or risperidone for behavior problems in dementia patients. These drugs don’t fix the dementia - they just suppress symptoms. And they raise the risk of stroke and sudden death. Benzodiazepines like diazepam (Valium) and zolpidem (Ambien) are also flagged for their link to falls and memory loss. Even some common painkillers, like long-term NSAIDs (ibuprofen, naproxen), are now listed as risky due to stomach bleeding and kidney damage.
Why Do These Drugs Still Get Prescribed?
It’s not because doctors are careless. It’s because prescribing for older adults is messy. Many have multiple conditions - diabetes, arthritis, heart disease, depression - and each doctor sees just one piece of the puzzle. A cardiologist prescribes a beta-blocker. A neurologist adds a sleep aid. A primary care doctor doesn’t always know what’s been given elsewhere.Polypharmacy - taking five or more medications - affects nearly 40% of older adults. And about 20% of them are on at least one drug flagged by the Beers Criteria. Some of these prescriptions started years ago and just never got reviewed. A patient gets a prescription for a muscle relaxant after a back injury in their 50s, and it keeps getting refilled into their 80s, even though they’re no longer active.
There’s also a cultural problem. Some doctors think, “If it’s not broken, don’t fix it.” But what’s not broken might be slowly breaking them. A sedative that helps someone sleep might be making them fall. A diuretic that reduces swelling might be making them dizzy. These side effects are often blamed on “getting old,” not on the medication.
How the Beers Criteria Are Used in Real Life
The Beers Criteria aren’t meant to be rigid rules. The AGS is clear: they’re a tool, not a mandate. They’re not supposed to be used to deny coverage or punish doctors. But they’ve become a benchmark.Hospitals use them to audit prescriptions. Pharmacists use them during medication reviews. Nursing homes are required to track how many residents are on Beers-listed drugs - it’s part of Medicare’s quality reporting. Some electronic health record systems now flag a Beers-listed drug the moment a doctor tries to prescribe it. That’s not a stop sign - it’s a pause. A reminder: “Did you consider alternatives?”
One study found that in patients stuck in hospitals waiting for long-term care (called ALC patients), 45.7% were on at least one Beers-listed medication. Once pharmacists stepped in and reviewed those prescriptions, many were safely stopped or switched to safer options. That’s not just theory - it’s saving lives.
And it’s not just about stopping drugs. Sometimes, the real problem is that a needed drug is being withheld because of fear. That’s where the Beers Criteria help too. They make it clear which drugs are dangerous - so doctors can feel confident using the ones that are safe.

What’s Different in the 2023 Update?
The 2023 version didn’t just tweak a few entries. It made major shifts based on new evidence:- Stronger warnings about antipsychotics in dementia - now listed as “avoid unless no other option and life-threatening behaviors exist.”
- Expanded guidance on benzodiazepines and “Z-drugs” - now clearly linked to increased fall risk, even at low doses.
- New criteria for drugs that raise fall risk - including certain antidepressants, antihypertensives, and anticholinergics.
- More precise kidney-based restrictions - not just “avoid if kidney disease,” but specific creatinine clearance thresholds.
- Added drug interactions - like combining NSAIDs with ACE inhibitors, which can cause sudden kidney failure.
These aren’t random changes. They’re based on real-world outcomes. Studies show that older adults on Beers-listed drugs are 30% more likely to be hospitalized for adverse events. The 2023 update tries to cut that number.
What About Other Tools Like STOPP-START?
You might hear about STOPP-START - another set of guidelines. The difference is simple: Beers tells you what to avoid. STOPP-START tells you what to avoid AND what to start.STOPP-START is great for catching missed treatments - like not prescribing a statin for someone with heart disease, or skipping a bone-strengthening drug after a fracture. But Beers is more widely used, especially in the U.S., because it’s simpler to track. Medicare and CMS use Beers for quality reporting. That means hospitals and pharmacies are more likely to have systems built around it.
They’re not competitors. They’re teammates. Many clinics use both: Beers to clear out dangerous drugs, STOPP-START to fill in the gaps.
How Patients and Families Can Use This Information
You don’t need to be a doctor to use the Beers Criteria. The AGS has free, easy-to-read versions on GeriatricsCareOnline.org and HealthinAging.org. You can download a pocket card, read the list, or even use the free mobile app.Here’s what you can do:
- Ask your doctor: “Is this medication on the Beers list?”
- Ask your pharmacist: “Can you review all my medications for risks?”
- Bring a list of every pill, vitamin, and supplement to every appointment.
- Ask: “Is this still needed? Can we try stopping it?”
Don’t stop a medication on your own. But do ask questions. Many older adults feel powerless when it comes to prescriptions. The Beers Criteria give you a language to speak up.
What’s the Big Picture?
The goal isn’t to eliminate all medications. It’s to make sure every pill has a reason. Every drug should be doing something important - not just sitting there, causing side effects.Deprescribing - the careful reduction or stopping of unnecessary drugs - is now a core part of geriatric care. And the Beers Criteria are the most trusted roadmap for that process.
It’s not perfect. Some patients need a Beers-listed drug because nothing else works. A person with severe agitation in dementia might need a low-dose antipsychotic for safety. Someone with chronic pain might need an NSAID if they can’t take acetaminophen. The criteria don’t ignore those cases - they just remind doctors to think twice.
The real power of the Beers Criteria is that they shift the conversation. From “What can we add?” to “What can we take away?” From “Is this helping?” to “Is this hurting?”
And that’s what matters most: making sure older adults aren’t just living longer - they’re living better.
Are Beers Criteria mandatory for doctors to follow?
No, the Beers Criteria are not mandatory. They’re a clinical guide, not a law. The American Geriatrics Society explicitly states they should never be used to punish doctors or deny coverage. They’re meant to support thoughtful, individualized care - not replace it.
Can over-the-counter drugs be on the Beers list?
Yes. Many common OTC drugs are on the list. Diphenhydramine (Benadryl), chlorpheniramine, and even some sleep aids and antacids are flagged because they have strong anticholinergic effects. These can cause confusion, constipation, dry mouth, and urinary retention in older adults - even at low doses.
How often are the Beers Criteria updated?
The American Geriatrics Society updates the Beers Criteria every three to five years. The most recent version was published in 2023. Each update is based on a review of hundreds of new studies, ensuring the recommendations reflect the latest evidence.
Do the Beers Criteria apply to everyone over 65?
Not always. The criteria are designed for most older adults, but exceptions exist. For example, someone with severe Parkinson’s might need a drug that’s normally avoided. The key is individualized judgment. The Beers Criteria help identify risks - but the final decision should involve the patient, family, and care team.
Can the Beers Criteria help prevent falls in older adults?
Yes. Several medications on the list - including benzodiazepines, antipsychotics, antidepressants, and some blood pressure drugs - increase fall risk. By reducing or replacing these drugs, the Beers Criteria directly help lower the chance of fractures and injuries from falls, which are a leading cause of death in older adults.




8 Comments
Pawan Chaudhary-17 December 2025
This is such a needed conversation. I’ve seen my dad on five different meds that just made him drowsy and wobbly. Once his pharmacist flagged Benadryl, everything improved. Simple swap, huge difference. Thanks for sharing this.
Jonathan Morris-18 December 2025
Let’s be real-the Beers Criteria are a bureaucratic tool disguised as clinical wisdom. The AGS doesn’t care about individual outcomes; they care about reducing hospital reimbursement claims. Every ‘avoid’ on that list has been weaponized by insurance companies to deny care. And don’t get me started on how EHR systems auto-flag safe prescriptions just to hit quality metrics. This isn’t medicine-it’s algorithmic paternalism.
Linda Caldwell-18 December 2025
My grandma was on Valium for 12 years because ‘it helped her sleep.’ We switched her to melatonin and a bedtime routine. She hasn’t fallen once in 18 months. This isn’t rocket science. Sometimes less is more. Start asking questions. You’ve got this.
Anna Giakoumakatou-20 December 2025
How quaint. The Beers Criteria-what a delightful anthropological artifact of 21st-century geriatric performative caution. One must wonder whether the AGS’s real agenda is not to optimize care, but to infantilize the elderly by pathologizing their very physiology. To prescribe anything at all is to admit that we’ve surrendered to the myth of biological determinism. The true liberation lies in embracing the chaos of aging-unmedicated, unfiltered, unapologetically frail.
BETH VON KAUFFMANN-21 December 2025
It’s statistically significant that 45.7% of ALC patients are on Beers-listed agents, but the real issue is the absence of standardized deprescribing protocols across care transitions. The criteria are descriptive, not prescriptive, and without structured clinical decision support integrated into EMRs, we’re just moving the deck chairs on the Titanic. Also, the 2023 update still lacks granularity on polypharmacy cascades-especially regarding CYP450 interactions with OTC antihistamines in renal impairment. A Band-Aid on a hemorrhage.
Raven C-23 December 2025
It is, of course, deeply tragic that the medical establishment continues to rely upon such reductive, quantitatively-driven heuristics-rather than embracing the profound, ineffable complexity of human aging. The Beers Criteria, with their sterile bullet points and algorithmic rigidity, represent not care, but the cold, bureaucratic commodification of frailty. One wonders: if a 78-year-old woman finds solace in a nightly dose of diphenhydramine, is it not our moral duty to honor her autonomy-even if it defies the cold calculus of evidence-based guidelines?
Donna Packard-24 December 2025
I work in a nursing home. We started using the Beers list as a checklist during med reviews. We’ve cut 30% of the high-risk meds without a single crisis. People are more alert. Fewer falls. Families notice. It’s not magic-it’s just paying attention.
Patrick A. Ck. Trip-25 December 2025
thank you for this post... i have a cousin who was on ambien for 7 years and no one ever thought to ask if she needed it... once we switched to light therapy and a consistent routine... she was like a different person. the beers criteria are not perfect... but they are a start. we need to talk more about deprescribing... and less about just adding more pills. sorry for typos... typing on phone.