When your eyes feel gritty, burning, or watery all at once, it’s not just allergies or fatigue. You might be dealing with dry eye syndrome-a condition more common than most people realize. It’s not simply about not having enough tears. It’s about the tears you do have not working right. And for millions, over-the-counter artificial tears are the first line of defense. But not all drops are created equal, and using them wrong can make things worse.
What Really Happens When Your Eyes Are Dry
Your tear film isn’t just water. It’s a three-layered shield: oil on the outside, water in the middle, and mucus on the surface. Each layer has a job. The oil keeps tears from evaporating too fast. The water hydrates and flushes out debris. The mucus helps the water stick to your eye. When any part fails, your eyes suffer. Most people think dry eye means not enough tears. But here’s the twist: 86% of cases aren’t about low tear production. They’re about tears evaporating too quickly because the oily layer is missing or broken. This is called evaporative dry eye, mostly caused by clogged meibomian glands-tiny oil glands along your eyelids. Think of it like a leaky car engine: you’ve got fuel (water), but no seal (oil), so everything burns off too fast. The other 10-15% have aqueous tear-deficient dry eye. This is when your lacrimal glands don’t make enough watery fluid. It’s often tied to aging, autoimmune diseases like Sjögren’s syndrome, or medications like antihistamines. Women over 50 are especially at risk, with nearly 70% of diagnosed cases being female. Symptoms don’t always match what you’d expect. Some people with severe dry eye report constant watering. That’s because the eye panics-when the surface is irritated, it overproduces watery tears that lack the right balance of oil and mucus. These tears don’t stick around. They just run down your cheeks.How Doctors Diagnose Dry Eye
There’s no single test. Diagnosis is a mix of symptoms, physical exam, and a few quick measurements. Your eye doctor might:- Use a strip of paper (Schirmer test) to measure how much tear your eye produces in five minutes. Less than 5mm means severe deficiency.
- Check tear break-up time-how long it takes for your tear film to dry out after a blink. Normal is 15-35 seconds. Under 10 seconds? That’s a red flag.
- Measure tear osmolarity with a device like TearLab. Healthy tears are around 300 mOsm/L. Above 308? You’ve got dry eye disease.
- Stain your eye with fluorescein dye to spot surface damage. Grades 3-4 on the Oxford scale mean serious, ongoing injury.
Artificial Tears: The Go-To Fix (But Not a Cure)
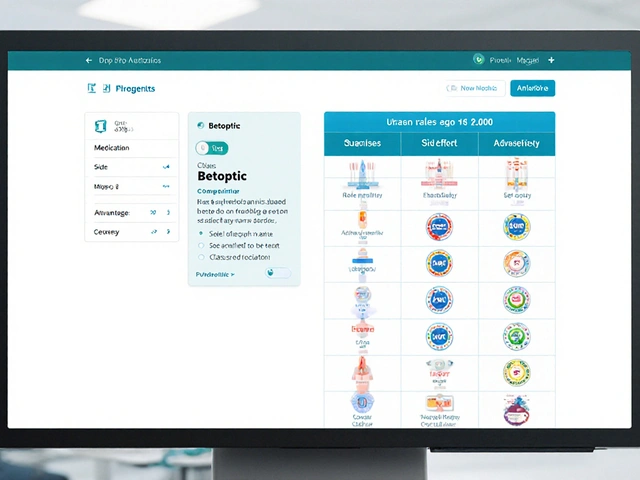
For mild to moderate dry eye, artificial tears are the most common solution. They’re designed to mimic natural tears, but not all are the same. The ingredients make all the difference. Most contain:- Electrolytes (sodium, potassium) to match your eye’s natural chemistry
- Viscosity agents like carboxymethylcellulose or hyaluronic acid to make the drops last longer
- Preservatives like benzalkonium chloride to keep multi-dose bottles sterile
Which Type of Dry Eye Are You? (And What Drops to Use)
If you have aqueous tear deficiency (not enough water), your best bet is a thick, electrolyte-balanced artificial tear. Look for formulas with hyaluronic acid or carboxymethylcellulose. Preservative-free is ideal if you’re using them 3+ times daily. If you have evaporative dry eye (oil layer broken), plain water drops won’t help much. You need something that adds back lipids. Products like Systane Ultra or Soothe XP contain lipid-replenishing ingredients. Some newer drops even include phospholipids to rebuild the oil layer. Many people don’t know which type they have. That’s why self-treating can backfire. If you’re using a water-based drop and your eyes still feel dry after 30 minutes, you might be missing the oil layer. Try switching to a lipid-enhanced formula for a week. You might be surprised.How to Use Artificial Tears Right
Using drops incorrectly is more common than you think. Most people:- Apply too many (2-3 drops when one is enough)
- Touch the dropper to the eye, risking contamination
- Don’t wait between different drops
- Tilt your head back slightly.
- Pull your lower eyelid down gently to form a pocket.
- Hold the bottle 1 cm above your eye. Don’t let it touch.
- Squeeze one drop in.
- Close your eye gently for 30 seconds. Don’t blink hard.
- If using another drop, wait at least 5 minutes.
When Artificial Tears Aren’t Enough
If you’ve been using drops daily for 4-6 weeks and still have:- Blurred vision that doesn’t clear
- Eye pain or sensitivity to light
- Corneal staining (graded 3-4)
- Difficulty wearing contacts
- Cyclosporine (Restasis) or lifitegrast (Xiidra)-prescription drops that reduce inflammation
- Punctal plugs-tiny devices inserted into tear ducts to keep natural tears on the eye longer
- Warm compresses and lid scrubs-for meibomian gland dysfunction
- New options like Eysuvis-a 2023 FDA-approved drop for flare-ups that works in minutes
The Future of Dry Eye Treatment
The dry eye market is growing fast-projected to hit $8 billion by 2030. Why? Because we’re all staring at screens longer. Average daily screen time is now 7.4 hours, and that increases dry eye risk by 28%. New treatments are on the horizon:- Lacritin protein therapy (Novartis)-in Phase 2 trials, aims to restore natural tear production
- Sustained-release hydrogel inserts-placed in the eye, dissolve slowly over 12 hours
- TrueTear neurostimulator-a tiny device that stimulates nerves to boost natural tears
- Microbiome treatments-targeting the bacteria on your eyelids that cause inflammation
What You Can Do Today
You don’t need a prescription to start feeling better. Here’s your action plan:- If you’re using drops 3+ times a day, switch to preservative-free single-dose vials.
- Try refrigerating your drops for longer-lasting relief.
- Use a humidifier at home, especially in winter or in air-conditioned spaces.
- Take screen breaks every 20 minutes. Look 20 feet away for 20 seconds.
- Apply warm compresses to your eyelids for 5-10 minutes daily to unclog oil glands.
- If symptoms last more than a month, see an eye doctor. Don’t wait for damage to happen.
Can artificial tears cure dry eye syndrome?
No, artificial tears don’t cure dry eye syndrome. They only manage symptoms by replacing or supplementing tears. They don’t fix the underlying causes like inflammation, meibomian gland dysfunction, or autoimmune issues. For long-term relief, especially in moderate to severe cases, treatments like cyclosporine, lifitegrast, or warm compresses are needed.
Why do my eyes water if I have dry eye?
This happens because your eye is irritated. When the tear film is unstable or evaporates too quickly, your eye sends a signal to produce more tears. But these reflex tears are mostly water-they lack the oil and mucus needed to stay on the eye. So they just run out, leaving your eyes still dry. It’s a sign your tear quality is poor, not that you have too many tears.
Are preservative-free artificial tears better?
Yes-if you use drops more than four times a day. Preservatives like benzalkonium chloride can damage the eye’s surface over time, especially with frequent use. Preservative-free drops, especially in single-dose vials, are safer and gentler for daily, long-term use. They’re also better for people with sensitive eyes or contact lens wearers.
Can screen time cause dry eye?
Yes. When you stare at screens, you blink 60% less than normal. Less blinking means your tear film doesn’t spread evenly across your eye, leading to faster evaporation. Studies show people with 7+ hours of daily screen time have a 28% higher risk of developing dry eye. Taking regular breaks and consciously blinking helps.
How long should I wait between different eye drops?
Wait at least 5 minutes between different eye drops. If you apply them too close together, the second drop will wash out the first one before it has time to work. This applies to artificial tears, prescription drops, and even eye drops for glaucoma. Waiting ensures each medication works properly.
When should I see a doctor for dry eye?
See an eye doctor if your symptoms last more than 4-6 weeks despite using artificial tears, or if you have blurred vision, light sensitivity, pain, or difficulty wearing contacts. If corneal staining is present (seen during an exam), it means your eye surface is damaged and needs more than drops. Early intervention prevents permanent changes.



12 Comments
Stuart Shield- 6 January 2026
Man, I used to think dry eyes were just from too much coffee and late nights. Then I started staring at code for 14 hours straight and suddenly my eyeballs felt like sandpaper wrapped in tissue paper. The part about evaporative dry eye? Mind blown. I’ve been using those cheap drops for years-turns out I’ve been putting water on a leaky boat. Switched to Systane Ultra last week and my eyes actually feel like they’re not trying to crawl out of my skull now. Who knew oil was the hero here?
Indra Triawan- 7 January 2026
It’s not just the eyes, you know? It’s the soul that dries out when you stare into the void of a screen all day. We are all just ghosts in the machine, blinking less, crying more, but never truly hydrated. The tears we shed are not for the pain-they are for the loneliness of being seen by no one, yet watched by everything.
Katelyn Slack- 8 January 2026
i just started using hyaluronic acid drops and my eyes feel so much better!! i had no idea about the oil layer thing… i thought it was just ‘dry’ like my skin. also i always touch the dropper by accident lol oops. i’ll try the 1cm thing now. thanks for the tip about refrigerating!!
Melanie Clark- 9 January 2026
Of course the pharmaceutical companies don’t want you to know that dry eye is caused by 5G radiation and fluoride in the water. They profit from selling you $40 bottles of placebo drops while your cornea slowly disintegrates. The ‘meibomian glands’? A distraction. The real cause is the government’s secret plan to make us all dependent on eye drops so we’ll stop looking at the truth. Watch your blink rate. They’re watching you. And yes, I’ve been using drops for 12 years. I’m still here. Barely.
Harshit Kansal-10 January 2026
bro i used to think my dry eyes were from being tired but turns out i was just a walking desert with eyelids. tried the warm compress thing last night-felt like a sauna for my face. woke up like a new person. also i stopped staring at my phone while brushing my teeth. small wins.
Brian Anaz-10 January 2026
Artificial tears? That’s what you call it? That’s just a Band-Aid on a bullet wound. America’s got the best eye doctors, the best tech, the best drops-but we still let people suffer because they’re too lazy to stop scrolling. You want relief? Stop looking at screens. Take a walk. Look at a tree. Or better yet-move to a country where people don’t live inside glowing rectangles. This isn’t medicine. It’s surrender.
Vinayak Naik-11 January 2026
as an optometry student in mumbai, i’ve seen so many patients who think ‘eye drops = cure’. one guy used 8 drops a day for 3 years and ended up with corneal ulcers. the real issue? no one checks the oil layer. we have a huge problem with meibomian gland dysfunction here-people think it’s just dust, but it’s their eyelids clogging like a greasy drain. warm compresses + lid scrubs = game changer. and yes, preservative-free drops are non-negotiable if you’re using them daily. i tell my patients: your tears are not tap water.
Saylor Frye-11 January 2026
How quaint. You’re all treating symptoms like peasants with a poultice while the real solution-neurostimulation, lacritin therapy, microbiome modulation-is already in Phase 3 trials. But no, let’s all keep buying $30 bottles of saline with hyaluronic acid because it makes us feel like we’re doing something. The irony? You’re all reading this on a screen. The system wins again.
Molly McLane-11 January 2026
Thank you for writing this with such care. I’m a teacher, and I spend 8 hours a day in front of a whiteboard and projector. My eyes felt like they were coated in plastic wrap. I started refrigerating my drops and using the 20-20-20 rule-and I swear, I can see my students’ faces again. Also, I told my class about blinking consciously. Now they all do it. It’s a tiny thing, but it’s a start. You’re not alone in this.
Wesley Pereira-11 January 2026
Let me guess-you’re using the $35 bottle with the fancy label and still wondering why your eyes feel like they’re being slowly boiled? Classic. You’re not ‘doing it right.’ You’re doing it like everyone else: half-assed. The 5-minute gap between drops? Nah, you’re slamming them in like a shot of whiskey. The dropper touching your eye? You’re basically giving yourself a bacterial tattoo. And don’t even get me started on the warm compresses-you’re probably using a damp washcloth from 2018. You want results? Treat this like a medical protocol. Not a hobby. Or keep crying into your keyboard.
Isaac Jules-12 January 2026
YOU’RE ALL WRONG. This isn’t about drops. It’s about the 5G towers installed in your apartment building. They’re drying out your tear film. The FDA knows. The WHO knows. But they’re letting you suffer because they’re profiting from your eye drops. I’ve been using a Faraday cage over my monitor and I haven’t needed drops in 9 months. Try it. Or keep buying placebo liquids from Big Pharma.
Pavan Vora-13 January 2026
I’ve been using artificial tears for over a decade, and I still can’t believe how much I didn’t know… the oil layer thing? I never thought of it like a car engine seal-brilliant analogy. I’ve been doing warm compresses with a boiled egg (yes, really-it’s what my grandmother taught me), and it helps more than any drop. I’ve also started using a humidifier in my bedroom-my eyes feel less like they’re trying to escape now. Thank you for this. I feel less alone.