Polypharmacy: When Too Many Medications Become a Risk
When someone takes polypharmacy, the use of five or more medications at the same time. Also known as multiple medication use, it’s not a diagnosis—it’s a situation that happens when different doctors prescribe drugs for different conditions, and no one steps back to see the full picture. It’s not rare. Nearly half of adults over 65 in the U.S. are on five or more prescriptions. And while each drug might make sense on its own, together they can create hidden dangers.
One of the biggest risks is medication interactions, when two or more drugs react in the body and cause unexpected side effects. For example, mixing a blood thinner like warfarin with certain painkillers can spike bleeding risk. Or taking a beta blocker like metoprolol with diabetes meds can hide low blood sugar symptoms. These aren’t theoretical problems—they show up in ERs every day. Another key player is adverse drug events, harmful reactions caused by medications, even when taken correctly. About 35% of hospital admissions in older adults are linked to these events, and polypharmacy is the top reason why.
It’s not just about the number of pills. It’s about how they work together. Some drugs slow down how your liver processes others, making them too strong. Others compete for the same receptors in your brain or kidneys. Grapefruit juice, for instance, can make statins or blood pressure meds dangerously potent. Even something as simple as a barcode scan in a pharmacy—meant to prevent errors—can’t catch every interaction if the prescribers didn’t communicate.
And it’s not just seniors. People with chronic pain, diabetes, heart disease, or mental health conditions often end up on multiple meds because each specialist focuses on their own area. But no one’s asking: "Is this too much?" Or "What happens if we take one away?" That’s where deprescribing, the careful process of reducing or stopping unnecessary medications comes in. It’s not about cutting drugs just to cut them—it’s about removing what doesn’t help anymore, or what’s doing more harm than good.
Some of the posts here show real-world examples: how metoprolol can mask low blood sugar, how grapefruit juice interferes with over 85 drugs, why stopping statins might be safer for some older adults, and how automated refills can accidentally keep you on meds you no longer need. These aren’t isolated cases—they’re symptoms of a system built to treat conditions, not people.
You don’t have to accept polypharmacy as normal. You can ask questions. You can bring a full list of everything you take—prescriptions, supplements, even over-the-counter pills—to one doctor who can review it all. You can ask: "Which of these is absolutely necessary?" "Could any of these be stopped?" "What happens if I stop one?" The answers might surprise you. And the right changes could mean fewer side effects, better sleep, less dizziness, and more energy.
Below, you’ll find real guides on how to spot hidden risks, understand why certain drugs clash, and learn how to talk to your doctor about reducing your pill burden. These aren’t theory pieces—they’re tools for people who are tired of taking too much and feeling worse for it.
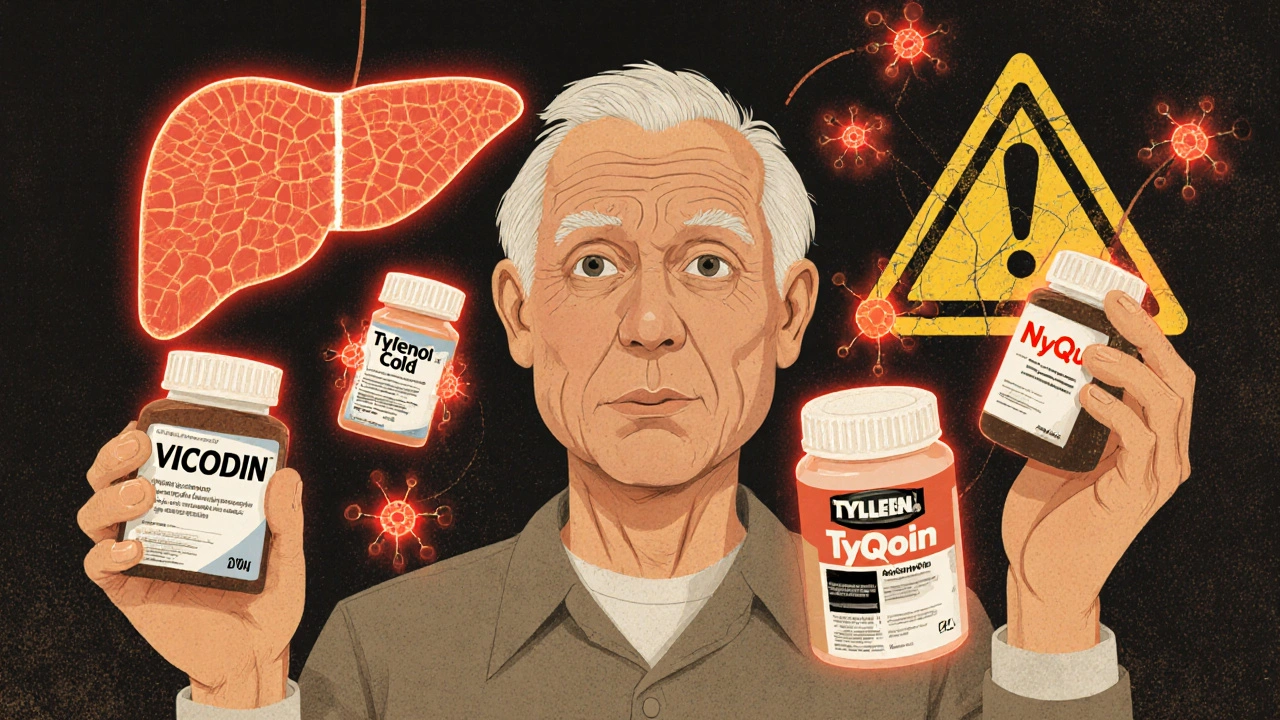
Safe Use of Multiple Medications: How to Avoid Dangerous Double Ingredients
Avoid dangerous double ingredients in your medications by knowing what’s in each pill. Learn how acetaminophen, diphenhydramine, and NSAIDs can cause overdose-even when taken as directed-and what steps to take to stay safe.
Deprescribing Frameworks: How to Safely Reduce Medications and Cut Side Effects
Deprescribing helps older adults safely reduce unnecessary medications to cut side effects, prevent falls, and improve quality of life. Learn how structured frameworks like Shed-MEDS and deprescribing.org tools make this possible.